 Testosterone Therapy for ED? That Depends …
Testosterone Therapy for ED? That Depends …
by Michael Jorrin, "Doc Gumshoe" | March 10, 2014 10:50 am
Doc Gumshoe looks at the latest on testosterone
[ed note: today we’re happy to publish the latest thoughts from “Doc Gumshoe”, who is a medical writer (not a doctor) whose work we often feature here at Stock Gumshoe — particularly because this piece is about one of the most heavily marketed cure-all supplements[1] out there for men of a certain age … which happens to be (on average) the same cohort as “men who buy investment newsletters”. As always, Michael’s words and opinions are his own … enjoy!]
The idea is appealing at first glance, no doubt. Among the many effects of testosterone is libido, so it would make sense that boosting testosterone would increase libido, and that would do wonders as a treatment for erectile dysfunction, wouldn’t it?
Lots of men seem to think so, as witnessed by the tripling of men getting testosterone supplements in the past decade. This has been a bonanza for the supplement manufacturers, and has also created a pipeline for the flow of serious money to certain celebrities who have been using their wide renown – or should we say notoriety? – to assist in the promotion of these supplements.
Who are they? Well, how many of us still remember Herman Cain? Poor Herman didn’t even come close to getting the nod back in 2012, but he emerged from that mêlée with at least one invaluable asset: an email list with about 360,000 names. And to that email list he has sent many, many messages boosting testosterone therapy, with such titles as “Breakthrough Remedy for ED!”
As usual with these mass emailings, you don’t just open the email and get a simple message – something clear and straightforward such as, “If you are experiencing erectile dysfunction, you might get some benefit from testosterone therapy.” Even skeptics like Doc Gumshoe wouldn’t find much to quibble about with a statement like that.
But no. You have to submit your name and email address, and Herman sends you a “cool, free report.” This turns out to be one of those interminable videos, which eventually reveals that the product that will cure your ED is called TestoMax 200, a product of Natural Breakthroughs Research, LLC.
Here, for your entertainment and amusement, is a bit from their website:
The Ultimate All-Natural Male Potency Booster?
There is a solution. Your desire can be boosted, your potency can be unlocked and reclaimed, using an all-natural 10 year-aged herb called found deep in the Indonesian rainforest, from farms that we personally work with. The highest quality, most potent extract is found in TestoMAX200:
It’s One Heck Of A Weird Trick.
Since I researched and released TestoMAX200, the world’s most potent all-natural male-mojo-boosting supplement, 99.6% of my clients over 48 report harder and longer lasting erections, more drive, assertiveness, and better action in-the-sack than they’ve experienced in over 17 years.
It is designed to lower your cortisol (stress[2] hormone) levels, as well as giving a major boost to your potency by increasing NATURAL testosterone production.
The men who have tried it are reporting an incredible difference in the way they feel and say their lovers are now seeing them in a completely different way. Like it was the first time again. Most of the stories we get are pretty X-Rated.
Reports include cases of:
- Large gains in performance
- Highly charged sex drive
- Verifiably increased muscle mass
- Visible gains in natural potency
- Actually feeling ALIVE again
But we don’t really have a lot of it left. Supplies are running out fast, and the next shipment of TestoMAX200 is held up for the next 4 months. When we run out, that’s it. It’s gone until we get more. And do you really want to be in the same place you are now, for even another 2 months?
I have not the slightest idea what that amazing herb (aged for 10 years) from the Indonesian rain forest might be – why can’t these magic herbs come from Kansas, I wonder? – but before we get anywhere near the pros & cons of testosterone supplements, we need to look at erectile dysfunction a bit more closely. The question that needs addressing is, how often is low testosterone – or “low T” as the advertising calls it – the real cause of ED?
The answer is sometimes, but by no means always.
What are some of the underlying causes of ED?
An erection is nothing more than blood flowing to the penis and filling the spongy tissue, which is what the penis mostly consists of. Usually all it takes is some physical and/or psychological stimulation, and the penis stays engorged with blood long enough to do the job. Therefore, anything that interferes with vascular function has the potential to result in failure to attain and maintain a satisfactory erection. What might some of these vascular obstacles be? Diabetes, heart disease, peripheral arterial disease, as well as obesity[3], smoking, and excessive alcohol[4] consumption. And those are just some of the factors that can result in ED.
It’s important for every man to be aware of those factors. Why? Because for many men, ED may be the first sign of a developing condition that could prove fatal. Therefore, the First Commandment regarding ED is DO NOT SELF MEDICATE!
As I was getting ready to send this piece off to be posted, a new major study popped up in my in-box, entitled “All Men with Vasculogenic Erectile Dysfunction Require a Cardiovascular Workup.” It lists 24 authors from 24 big-time academic and medical institutions in the US, UK, France, Italy, and Greece[5]. The premise is that if the source of the problem is not psychological, then it’s vascular – something interfering with blood flow.
Here’s a bit directly from the paper:
“An emerging paradigm indicates that erectile dysfunction is, in fact, an independent marker of cardiovascular disease[6] risk. Thus, the presence of erectile dysfunction may provide the opportunity for cardiovascular disease mitigation in men with otherwise unrecognized cardiovascular disease.” (Miner M et al, Am J Med 2014)
In many cases, dealing with the underlying cause will also bring about resolution of the ED, although sometimes not right away. Many men with ED develop a degree of performance anxiety. Having failed to get and keep a satisfactory erection, the fellow loses confidence in his ability to perform next time and the time after that. It’s the equivalent of a batting slump, and he may benefit from a coach that helps him get the kinks out of his swing.
"reveal" emails? If not,
just click here...
The warning about self-medication applies not only to testosterone-boosters but to the Viagra-type medications. These are drugs of a class called phosphodiesterase (PDE5) inhibitors, and they work by relaxing the blood vessels to the penis and also the spongy tissue, permitting them to fill with blood. This is accomplished by inhibiting the activity of a substance that makes the erection go away.
However, in some men PDE5 inhibitors are absolutely contraindicated. This would include men (I say “men” because it’s usually men, but the contraindication would apply to women as well) with angina who are taking nitroglycerine or nitrates. Both the angina drugs and the ED drugs have a short-term powerful blood-pressure lowering effect, and doubling this effect could prove dangerous.
Perhaps more important than the potential for harm with these agents is the need for men to discuss the implications of ED with a physician, in spite of the understandable reluctance of proud, manly, virile males to broach the subject. Doc Gumshoe would be remiss if he didn’t put in capital letters and bold type that ERECTILE DYSFUNCTION IS NOT USUALLY A SIGN OF DECLINING MANHOOD! Guys should swallow their embarrassment, own up to their physician, and do whatever it takes to get to the root cause – because, if it’s one of those conditions I mentioned above, detecting the cause of ED could mean early and effective intervention in a progressive disease with potentially grim consequences.
But, yes, low testosterone can be a factor in ED.
Testosterone, I’m sorry to say, declines steadily with advancing age, so in older men libido may decline and the potential for ED increases. Thus, along with other factors, “low-T” can lead to ED. In younger men, however, low testosterone has other causes, ranging from kidney, liver, and pituitary diseases, trauma to the testes, and hemochromatosis, a condition in which people absorb too much iron from their food, which affects testosterone levels. Even contracting the mumps after adulthood. As with the vascular causes of ED, low testosterone, particularly in younger men, requires further investigation before boosting testosterone with supplements or prescriptions.
It’s not a problem, it’s an opportunity!
… or, perhaps I should say, that’s how it’s viewed by the marketers of testosterone boosters. Reliable surveys report that about one fifth of men between 50 and 60 have some ED, and slightly more than half of men older than 65 have some ED. In all, close to 20 million men in the US have some ED.
That’s a big market. The PDE5 makers have done and will doubtless continue to do just fine in that market. But PDE5s by themselves don’t deliver the whole package. For one thing, they do not boost libido. And testosterone has a range of other effects that most men would consider desirable – for example, boosting testosterone increases lean muscle mass and strength, as well as bone density, at least in some men. In that sense, it has a lot of the hallmarks of the “Fountain of Youth” elixir.
And sales of testosterone-boosting supplements have increased dramatically in the past 10 years. One recent study, looking only at prescriptions for testosterone supplements – not at sales of substances, whether Indonesian herbs of others, that are promoted to boost testosterone – found a three-fold increase between 2001 and 2011. Here are the figures:
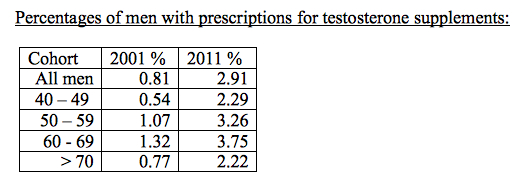
The fastest rate of increase, about five-fold, was in testosterone gels. But slightly less than a third of the men (31.88%) were prescribed testosterone specifically for ED. The indication for which testosterone was most often prescribed was hypogonadism, which is more or less synonymous with low testosterone. However, not all the men for whom testosterone was prescribed had their testosterone levels assessed. (Baillargeon J et al, JAMA Int Med 2013)
So, what’s the problem?
Well, there are at least a couple of problems.
Problem one is that if low testosterone is not the most frequent underlying cause of ED, and if instead the most frequent causes are conditions that could progress to being genuinely life-threatening, then testosterone therapy could amount to ignoring the first signal of a serious disease.
Problem two is that there is at least a strong possibility that among the many effects of testosterone is that it increases the progression of prostate[7] cancer, so testosterone therapy of any kind could be a genuinely dreadful idea. This is based on evidence that stopping the production of testosterone also halts – usually! – the progression of prostate cancer. On the other hand, evidence that testosterone supplementation actually accelerates the progression of prostate cancer is equivocal. But acquiring such evidence would be hugely problematic. Is there going to be a clinical trial in which men with confirmed early stage prostate cancer are given testosterone in order to determine whether their cancers grow more quickly? I don’t think so.
The accepted wisdom is that although testosterone may speed the progression of prostate cancer, it does not actually cause prostate cancer. Hearing that, I hear the spirit of Miss Truesdell telling me to think for a moment.
What we know about cancers of any kind is that mutant cells are constantly popping up in our bodies, like dandelions in a spring lawn. Our immune system fortunately wipes out the great majority of these little mutant cells, before they develop into cancers, which is what they are aiming to do. What that means is that huge numbers of men have early stage prostate cancers, many or most of which will not progress to the point where they do serious harm. (We know this, by the way, based on well-publicized autopsy records that show that most men who live into their senior years die with, but not of, prostate cancer.)
So, if lots of men have those early stage prostate cancers, why in the world would any man want to submit himself to a mode of therapy that could accelerate the growth of a relatively indolent cancer, transforming it into an aggressive, perhaps deadly cancer?
And, by the way, testosterone treatment is contraindicated by the FDA[8] in men with a diagnosis of either prostate or breast cancer.
Another bit of information to add to this scenario is that a form of treatment for prostate cancers that do not respond to usual treatment, that being surgery[9] or a form of radiation, is castration. This is sometimes accomplished chemically, by administering a drug that effectively stops the secretion of testosterone from the testes. Chemical castration is sometimes used in men with locally advanced prostate cancers as an alternative to surgery or radiation.
And sometimes it is accomplished surgically – the procedure is termed orchiectomy. When, during surgery for prostate cancer, the cancer is detected as having spread to the lymph nodes, the surgeon will often (with the patient’s prior consent) remove the testes to attempt to prevent further spread of the cancer.
Is there other information that can help us figure this out?
A starting point needs to be an understanding of the overall physiologic function of testosterone. It’s not just a hormone that promotes sexual activity. Testosterone is essential to a great many body functions, including muscle and bone development – not just the primary and secondary male sexual characteristics. And, yes indeed, low testosterone is associated with a range of important deficits in bodily health.
First, low testosterone is highly correlated with obesity. A very large study found that as BMI increased in a cohort of men from less than 25 to greater than 35 kg/m2 – i.e., from the weight category considered normal to obese, hypogonadism essentially quadrupled. Depending on what testosterone levels were used to define hypogonadism, the prevalence of hypogonadism in obese men was as high as 60%.
Remember, this is a correlation, so we can’t assume that one condition causes the other. The proponents of testosterone therapy as the magic elixir that brings youth and strength and health would likely argue that obesity follows from “low T,” and that boosting testosterone would increase activity and help combat obesity. It’s an appealing premise, but the data supporting it is far from conclusive.
Low testosterone is also correlated with shorter life expectancy, both in patients with cardiovascular disease and type 2 diabetes[10]. Again, this is a correlation. But the studies to determine whether boosting testosterone increases life expectancy in patients with those conditions are far from conclusive. One study (Vigen R et al, JAMA 2013) actually found a slightly increased risk – about 5.8% – for total mortality, heart attacks, and strokes, in men who received testosterone therapy; however, this study has been challenged on the basis of methodology. Another study found that testosterone therapy in men with type 2 diabetes who had very low testosterone levels reduced the mortality risk from 19.2% to 8.9% at the end of 80 months. This was not a randomized, controlled study, but a retrospective analysis of a large group of men treated in a diabetes clinic. (Muraleeldharan V et al, Eur J Endocrinol 2013).
A study that has received considerable notice, including an Op Ed mention in the New York Times arrived at a contrary result. It enrolled 209 men, average age 74, and compared the effects of testosterone versus placebo for 6 months, at the end of which 23 men in the testosterone group and 5 in the placebo group had had adverse CV events – none fatal, most non-serious. The subjects all had low baseline testosterone as well as physical mobility limitations, most were hypertensive, and about half had pre-existing cardiac conditions. The testosterone group experienced significant improvements in mobility and strength. The study authors formed no general conclusions about testosterone therapy and were cautious about ascribing the adverse events in this trial to testosterone. (Basaria G et al, N Engl J Med 2010) I point out that this was a very short study, and it’s possible that increased physical capacity in the treatment group might have resulted in reduced cardiac risk over a longer term.
The testosterone/prostate cancer link is the most challenging one to parse. At least one highly responsible physician who prescribes testosterone does so only after carrying out prostate biopsies to rule out the possibility of occult prostate cancers.
However, in men with very low testosterone, referred to in the literature as “near castrate” levels, testosterone therapy results in small increases in levels of prostate-specific antigen, or PSA. In men with somewhat higher testosterone levels, adding more testosterone to the mix seems to result in less significant increases in PSA, and, it is assumed, a lower risk of fueling the progression of prostate cancers. One eminent urologist, Abraham Morgentaler, concludes that while there is ample evidence that lowering testosterone causes prostate cancer to regress, increasing testosterone does not appear to cause prostate cancer to progress more rapidly (Morgentaler A, Eur Urol 2006)
(I am not stating what the numerical values for low versus normal testosterone might be. In various studies, they are expressed in different ways, ranging from nanograms per deciliter to nanomoles per liter. And there are several ways of measuring testosterone, further confusing the picture for the general public.)
The basic question: does testosterone therapy reliably treat ED?
The intuitive response would be, “It’s bound to.” But, as with most of this, the evidence is conflicting. Some studies say yes, some say no. The study that I find most persuasive, in men who did not respond to tadalafil (Cialis), reported that in men with normal or high baseline testosterone levels, there was no significant benefit in terms of improvement on the International Index of Erectile Function (IIEF) scale. But with lower baseline testosterone levels, scores in men receiving testosterone supplements were triple those in patients receiving placebo, and in men with very low testosterone levels, the IIEF scores were five times higher than in the placebo group. (Buvat J et al, J Sex Med 2011)
Another encouraging study, this one only in men with low baseline testosterone levels who had failed to achieve successful response with sildenafil (Viagra), reported that 34.3% got a satisfactory response with added testosterone. Then, in those men who had not responded to testosterone alone, sildenafil was added to the regimen, and 37.5% of that group attained a satisfactory response with the combination of sildenafil and testosterone. (Hwang TI et al, Int J Impot Res 2006)
Late breaking …
As I was preparing to send this off to Travis to be posted, Endo Pharmaceuticals (ENDP) announced that their testosterone supplement, Aveed, just got FDA approval after three turn-downs – first for safety concerns, and then two more because their risk-mitigation plan wasn’t thought to come up to snuff. Aveed is given by injection at 10-week intervals. The market leader, by the way, is AbbVie’s (ABBV) AndroGel, a testosterone gel, as the name implies. An interesting option is Auxilium’s (AUXL) TestoPel, consisting of testosterone pellets implanted under the skin. There are lots, and there will be more.
So where do we come out?
Sifting through all this information, it seems to Doc Gumshoe that some fairly clear conclusions emerge:
- One: no self-medication.
Testosterone therapy should not be undertaken except under the supervision of an experienced physician, and only after confirmation that the patient does indeed have levels of testosterone that are significantly lower than expected for a man of his age. - Two: keep an eye on prostate cancer.
Even though the data on whether testosterone does or does not speed the growth of prostate cancer is conflicting, candidates for testosterone therapy need to be monitored carefully for prostate cancer, whether by regular PSA tests or needle biopsies. - Three: consider testosterone for other conditions as well as ED.
Testosterone therapy may bring benefits not only to men with erectile dysfunction, but to men with diabetes or cardiovascular disease – always with the proviso that they have confirmed low baseline testosterone levels. - Four: be careful of “natural” testosterone boosters.
In the absence of conclusive evidence, “natural” testosterone boosters should be managed with the same care as prescription testosterone products.
* * * * * * *
Doc Gumshoe concedes that this one was tough. I think most men would like to believe that just a touch of the old stuff (that we used to manufacture ourselves with no problem at all!) would return us to our 20-year-old selves. Well, not so fast! At the same time, my guess is that there are very real benefits, and that the science is a long way from being all wrapped up. I’ll try to keep you posted as things develop. In the meantime, on the other side of the aisle, what’s the story on hormone replacement therapy for post-menopausal women? We now understand that it’s not the panacea that it was hyped to be, but has it been totally, entirely discredited? Doc Gumshoe will apply Miss Truesdell’s methods to that controversial topic in a future piece. In the meantime, keep the comments coming – thumbs up or thumbs down. Best to all, Michael Jorrin (aka Doc Gumshoe)
- supplements: https://www.stockgumshoe.com/tag/supplements/
- stress: https://www.stockgumshoe.com/tag/stress/
- obesity: https://www.stockgumshoe.com/tag/obesity/
- alcohol: https://www.stockgumshoe.com/tag/alcohol/
- Greece: https://www.stockgumshoe.com/tag/greece/
- cardiovascular disease: https://www.stockgumshoe.com/tag/cardiovascular-disease/
- prostate: https://www.stockgumshoe.com/tag/prostate/
- FDA: https://www.stockgumshoe.com/tag/fda/
- surgery: https://www.stockgumshoe.com/tag/surgery/
- diabetes: https://www.stockgumshoe.com/tag/diabetes/
Source URL: https://www.stockgumshoe.com/2014/03/testosterone-therapy-for-ed-that-depends/
I find it strange that neither in Michael Jorrin’s otherwise excellent report nor in the comments afterward was it mentioned that introducing artificial testosterone (in any form) results in the body slowing down and stopping its own testosterone production, causing a permanent dependence on the artificial replacement. Any comments?