[Ed note: if you’re new to Doc Gumshoe, this is our break from investment chatter: He’s our favorite medical writer and he shares his contrarian and thoughtful commentaries with us every now and again. Any opinions and assertions are his own.]
It all starts with an unassailable truth: the healthier you are to start with, the better your odds of fighting off a whole range of illnesses, from Addison’s Disease to Zollinger-Ellison syndrome. The essentials of staying healthy are not deeply mysterious, and if I listed them here, you would likely emit a groan and move on to something more interesting. But another truth, unfortunately also unassailable, is that for most of history, the emphasis in mainstream medicine has been not on keeping people healthy, but on treating sickness. People go to the doctor, not when they want advice on how to stay healthy, but when they are sick. The first medical question the doctor wants an answer to is, “what’s your principal complaint?” If you don’t have a principal complaint, why are you here?
Yes, there have always been wise doctors who stressed staying healthy, and recently health maintenance has been increasingly emphasized by all manner of medical bodies – government, academic, professional organizations, and voluntary groups. Take high blood pressure – hypertension – as an example.
The JNC7 Catechism
The Joint National Committee on Prevention, Detection, Evaluation, and treatment of High Blood Pressure (widely known as the JNC) has, in its past several treatment recommendations, emphasized “Life Style Modifications” as the treatment for persons having what they now term “prehypertension.” Here’s how they classified blood pressure in their latest recommendations:
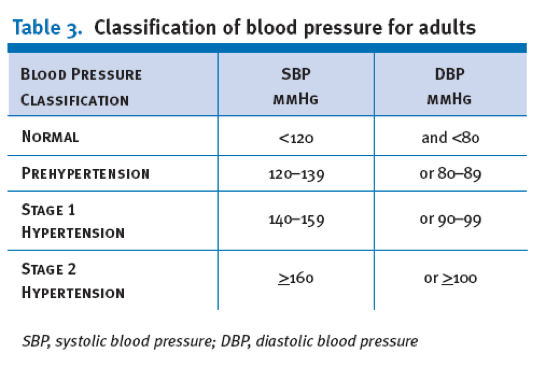
[The Seventh Report of the Joint National Committee on Prevention, Detection Evaluation, and Treatment of High Blookd Pressure. JAMA 2003;289:256-71]
And here’s how they say prehypertension needs to be treated:
“Prehypertension is not a disease category. Rather, it is a designation chosen to identify individuals at high risk of developing hypertension, so that both patients and clinicians are alerted to this risk and encouraged to intervene and prevent or delay the disease from developing. Individuals who are prehypertensive are not candidates for drug therapy based on their level of BP and should be firmly and unambiguously advised to practice lifestyle modification in order to reduce their risk of developing hypertension in the future (see Lifestyle Modifications).”
This is what they say about Lifestyle Modifications:
“Adoption of healthy lifestyles by all persons is critical for the prevention of high BP and is an indispensable part of the management of those with hypertension. … BP is also benefited by an adoption of the Dietary Approaches to Stop Hypertension (DASH) eating plan, which is a diet rich in fruits, vegetables, and lowfat dairy products with a reduced content of dietary cholesterol as well as saturated and total fat. … Dietary sodium should be reduced to no more than 100 mmol per day (2.4 g of sodium). Everyone who is able should engage in regular aerobic physical activity such as brisk walking at least 30 minutes per day most days of the week. Alcohol intake should be limited to no more than 1 oz (30 mL) of ethanol, the equivalent of two drinks per day in most men, and no more than 0.5 oz of ethanol (one drink) per day in women and lighter weight persons. … For overall cardiovascular risk reduction, patients should be strongly counseled to quit smoking.”
What Happens in the So-Called “Real World”
So here’s what happens, at least quite a lot of the time: our patient walks into the doctor’s office, and his blood pressure is 135 over 85. (I made our patient a man, because men are more likely to have high blood pressure than women.) The doctor tells him, without a whole lot of conviction, that he has “prehypertension,” and that he needs to do some lifestyle modification. (I should note here that the concept of “prehypertension” has not had a lot of take-up in the clinical community; most docs have a reasonably good notion of which of their patients are at higher risk for developing established hypertension and which ones can continue in the “prehypertension” range without progressing to the real thing.)
Our patient already knows what’s coming: more exercise, less yummy food, less booze, no smoking. He knows he should follow that plan, and he hopes he’ll have the strength of character to, by gosh, just do it! And maybe, at first, he sort of does follow it. But the problem is, he feels absolutely fine. He has no symptoms, and therefore no regular incentive to stay with the program.
Okay, a year or two later he’s back at the doctor’s, and now his BP is 150 over 95, and the doc tells him that he now definitely does have hypertension. The doc asks him, perhaps more out of duty than really wanting to know, whether he has stuck with his lifestyle modification plan. Maybe he weasels, maybe he fesses up. The doc knows, however, that the chances are that our guy has not stuck with the plan. So now the doc tells our patient that he has got to get on that plan and stick with it, and he’s going to prescribe an antihypertensive drug to go along with it.
Now he’s facing the prospect of being on an antihypertensive drug for the rest of his life. Or maybe two, or even three different antihypertensive drugs.
The Alternative Treatment “Solution”
Then, this pops into his in-box:
“SECRET REVEALED: Lower Your Blood Pressure
Without Medication”“How to Lower Blood Pressure Naurally Once & For All!”
“Top-Secret Ingredient From the Deep Sea Found to
Naturally Lower Blood Pressure
& Cholesterol Without Expensive Prescriptions!”
Skipping down a bit, there’s this …
“Big Pharma and conventional regimens will have you confused, over-medicated, and frustrated because you aren’t treating the major triggers of elevated blood pressure.
Not only do you lose time and money, you end up losing faith that there are answers.
Here’s the secret: you lower your blood pressure by reversing the major triggers of elevated blood pressure at the cellular level … and by inhibiting the #1 Blood Pressure Enzyme.”
Of course, there’s a link to a video, which starts off with this banner headline:
“Deep Sea Secret Scientifically Proven
to Fight Real Cause of High Blood Pressure
Watch Below for Revealing New Evidence”Are you getting our free Daily Update
"reveal" emails? If not,
just click here...
Then follows a little line warning you that the 25% savings expires tomorrow. No matter when you click on the link, the 25% savings always expires tomorrow.
The video continues:
“I want you to forget every depressing thing you’ve ever heard or believed about getting older…
Think living to 120 in great health & a good mind is impossible?
(Not Anymore!)There’s an astonishing new breakthrough from the deep sea that’s changing the very “facts of aging” … it has the ability to restore nearly every part of your body to a younger, stronger, and more rejuvenated state… making you virtually immune to the diseases of “old age!”
Our Bottom Line Scientific Facts Will Show You How Studies Reveal The Secret To:
- Lower bad oxidized LDL cholesterol by over 29 points!
- Improve blood flow by over 50% and revive damaged arteries!
- Cut your odds of dementia by almost half!
- Safeguard your eyes for lifelong healthy vision!
- Boost brain energy levels by a staggering 71%!
Here’s One Thing I Need You To Do Before We Go Any Further… Turn off the TV– your Cell Phone, close down your email and… LOCK the door & Pay Attention to Every Word on This Page.
Okay. The video goes on and on, and eventually – eventually! – it reveals what the ingredients are in this amazing miraculous cure:
The first is …
“Seanol™: An extremely rare seaweed extract (from Ecklonia Cava) proven 100 times more powerful than any land-based antioxidant.
Over 15 years of research and nearly $40 million worth of clinical studies back it up.
It’s the only FDA-approved Ecklonia Cava marine-algae extract in existence.
Not Only is Seanol More Potent… It Stays In your body 12 Hours, compared to Land Based Antioxidants that work on for 30 minutes…”
The second is …
“Super Ingredient #2:
Calamarine™:A deep-sea omega-3 discovery that blows away every fish oil in existence!
It delivers an unheard of 85% more DHA omega-3s to your heart, brain, joints, and eyes!
Scientists have discovered that the type of omega-3 it contains is the true miracle worker.
Not only is this the worlds most powerful Omega…
But you can get more than 8X the benefits of a Fish Oil without the burps and after taste…People LOVE This Benefit…
With This SUPER-OMEGA, you can say goodbye to your fish oil and…
- Fatigue
- Heart trouble
- Poor memory
- Vision Problems
- Dry or itchy skin
- Joint pain
- Lack of endurance
- Poor circulation
- Mood swings or depression”
… and the third is …Vitamin D3!
“For The 1st Time Ever, These 2 MARINE SUPER NUTRIENTS Have Been Combined For YOU!
It’s never been done before, but we’re bringing you the first age-busting formula that combines Seanol and Calamarine.
It’s called Marine-D3.
Why D3?
Because it also includes a superior form of vitamin D…
To Give You Even MORE Intense Rejuvenation & Repairing POWER!
Research shows that this life-saving vitamin plays a key role in preventing nearly every major disease, from depression to heart disease.
But a whopping 75% of Americans simply don’t get enough!
Your cells are literally starving to death without it!
With Marine-D3, turning back the clock is no longer some futuristic dream – it’s a longevity breakthrough you can benefit from NOW!
Its Extreme Rejuvenating Power Comes From Joining Three Healing Powerhouses!
Each of these nutrients is tremendously effective on their own, but when combined for the first time ever in Marine- D3, the synergy of all three delivers unprecedented anti- aging and disease-fighting benefits!
Together, they attack aging from every conceivable angle and restore health in nearly every system in your body!”
Well, we can easily see why our patient would be sorely tempted by these blandishments – live to 120 in good health, why not? And the ingredients in this remedy all sound on the up-and-up – an antioxidant, a source of Omega 3, and Vitamin D3. These couldn’t be bad, and who knows, they might even help with his hypertension.
For the moment, I won’t go into the reservations that have been raised about the effectiveness of antioxidant supplements. I will do no more than suggest that those evil free radicals that they’re supposed to counteract may indeed have some necessary function, and that perhaps we shouldn’t be in a hurry to extirpate then utterly. (There will be more about that in a future commentary.) But here’s the issue:
Will Supplements That Contribute to Health Actually Cure an Illness?
We’re in agreement that the better a person’s baseline health, the better his or her chances are of warding off all manner of illness and disease. But once that disease raises its ugly head, will taking steps that contribute to overall health do much to reverse the course of the disease?
Let’s go back to high blood pressure as an illustrative case. The pathophysiology (medicalese for the processes that lead to the illness) of hypertension is complex, and I’m sure you don’t have the patience for a digest of Braunwald’s 2000 page Heart Disease text. But let me present a simple example of a common cause of high blood pressure, and try to explain how it plays out.
Suppose a person eats a really salty meal. Here’s what happens: first, the concentration of salt in his (yes, it’s a guy again!) blood stream rises. As the blood passes through the kidneys, a precise regulatory process takes place. The sodium concentration in the blood needs to be kept at a constant level, so if it gets too high, the blood needs to be diluted by adding water – i.e., our patient gets very thirsty, drinks water, and the total fluid in his blood stream increases. But the total capacity of his circulatory doesn’t increase, so what happens is that the blood is under greater pressure – i.e., hypertension. Now, this hypertension could be temporary. The kidneys will then pass the excess liquid from the blood into the bladder, and into the toilet it goes, restoring our patient’s BP back to where it was before he scarfed down all those salty snacks.
During that interval, while he was having an episode of hypertension, warning signals were being sent from his circulatory system to his brain. Most large arteries have nerves which sense the pressure within the artery; these are called baroreceptors. The way they work is that when pressure increases in the artery, it stretches to accommodate the pressure, and the nerves stretch, and they send signals to the brain stem saying, “Do Something!” The brain then sends signals that reduce heart rate and relax arterial muscle tone, lowering blood pressure.
These baroreceptors work very well indeed, but for a short time only. When there are rapid changes in blood pressure, the signals go off quickly, at really short intervals. However, their function is short-term modulation of blood pressure. After as short a time as a couple of days, if blood pressure remains elevated, the baroreceptors stop sending these alarm signals, and accept the increased BP as the ”new normal.” This phenomenon is sometimes called “resetting the barostats.”
What that means is that if our patient regularly overloads on salt, his body essentially has no way of sensing that he has high blood pressure. His kidneys will do what they need to do to keep his sodium level at an okay concentration, but as far as blood pressure regulation, his brain now accepts that 150 over 95 is normal. It’s getting no alarm signals from the baroreceptors.
Other Mechanisms of Hypertension
I don’t want to leave you with the impression that every time you eat potato chips, you’re risking a lifetime of drug treatment for high blood pressure. Some people are more salt-sensitive in this regard than others; that seems to be particularly the case in people who are genetically programmed to retain salt, perhaps because their ancestors lived in parts of the world where salt was scarce. Another common mechanism is the renin-angiotensin system (RAS). Renin is an enzyme produced by the adrenal glands, adjacent to the kidneys. Renin eventually becomes a substance called angiotensin, which promotes constriction of the arteries, increasing BP, and boosts the heart’s pumping action, also raising BP. Some individuals are more renin-sensitive than others and therefore more prone to hypertension.
There are many effective and (by and large) quite safe drugs to treat hypertension. I’m not going to try to evaluate the different classes at this point, but if you would like to hear my personal views, please post a comment to that effect and I could devote a piece to those issues.
However, the bottom line here is that once hypertension is established, changing the lifestyle factors that led to hypertension isn’t going to do much to make it go away. Disease processes are in place, and these need to be attacked directly.
But What About Those Healthful Supplements?
Okay, that particular combination consisted of three ingredients, all of which actually do have some healthful credentials.
First, antioxidants. There is some evidence suggesting a connection between oxidative stress and factors that increase blood pressure, and at least one study reported that some hypertensive patients that took a supplement, pycnogenol, based on pine bark, were able to reduce the dosage of their antihypertensive drug by about 30% without their BP rising significantly. But so far data about this association is scant, and antioxidants vary all over the map, so on this front my guess is that treatment for hypertension with antioxidants of any kind is a shot in the dark. And data on the antioxidant in the “Marine D3” preparation, ecklonia cava, is slim.
Second, Omega 3 supplements. These do have a beneficial effect on lipid balance. They tend to raise HDL cholesterol (the good kind), lower triglycerides, and have a small effect on LDL cholesterol (the bad). People with elevated cholesterol frequently also have high blood pressure, but the two conditions need to be treated separately – fixing one doesn’t fix the other, so I don’t see Omega 3’s as an effective high blood pressure remedy.
Third, Vitamin D. Here the story is more interesting. There is strong evidence that persons with low levels of a hormone (calcifediol) which is metabolized in the liver from Vitamin D3, have increased cardiovascular mortality and increased prevalence of hypertension. The suggested mechanism is that Vitamin D3 may inhibit the RAS, through which heart rate and arterial pressure are increased. So you would think that taking supplemental Vitamin D3 might actually lower blood pressure. However, so far, evidence that it actually works as a treatment for hypertension is absent.
My bottom line: these supplements might well help to maintain health, but they’re highly unlikely to control established high blood pressure. Staying healthy and treating disease are two separate projects, and each one has to be addressed individually. This is not only true for hypertension, but for most other diseases, despite the rosy pictures painted by the merchants of alternative treatments.
* * * * * * * *
Let me remind you – “Doc Gumshoe” is not a physician. I’ve been a medical writer for 30 years or so, and, while I stick up for my capacity to understand the medical evidence as well as anybody else, I don’t give specific medical advice. Physicians treat human patients; I deal in scientific (I hope!) information. I am exceedingly grateful for any kind of feedback and can try to address specific questions. And if there are general topics that you would like to hear more about, please let me know!
Michael Jorrin (aka Doc Gumshoe)
 Is There a Common Theme in Alternative Medical Therapies?
Is There a Common Theme in Alternative Medical Therapies?
A personal note on Vitamin D: I am well into my seventies. Recently I came under the care of a new urologist. The first thing I told him was “I started having calcium kidney stones over 50 years ago – passed most. However, I’ve had virtually none – certainly no large ones – for at least five years since an Endocrinologist had me take a once/week Vitamin D pill containing 50,000 I.U.”
He raised his eyebrows, shook his head and could not explain the reason for those results.
I’m still on the Vit. D. every Monday.
Please don’t bother telling me it’s a coincidence. Any observations or suggestions however WILL be appreciated.
God bless us all and especially YOU, Travis.
I have been taking anatabine as anatabine citrate (trade name Anatabloc) in the unflavored tablet 3 daily and have had these results: BP dropped from 140/90 to 118/65( meds got it to130/80); an arthritic trigger finger is now fine which the chiro and the ortho docs said they couldn’t totally fix; a varicose vein in my foot no longer swells; an inflammatory bowel situation no longer has me living close the the bathroom. I know the improvements in these conditions are not cures as all the symptoms return when I am off my 3 daily for a week or so. And I know that this could be a sort of drug therapy, just not identified by Big Pharma just yet. Anatabine is from the tobacco plant which doesn’t necessarily make it a bad product. I would be interested in natural ways to reduce chronic inflammation from a lifestyle viewpoint or other natural ways. Anatabloc has anti-inflammatory effects.
Bravo Travis….nothing like an article like this to bring out some strong responses. I am firmly in the camp of “good science” when it comes to medical and health issues…although knowing which is “good” and which is “bad” science is always a challenge. Most things I see or read appear to me to be based on conspiracy theories of one sort or another….drug companies, “big pharma”, doctors in collusion with….etc. etc. I feel pretty safe rejecting any of those sorts of pitches immediately. But it is hard to find good balanced consensus science based information sometimes because no one really makes a lot of bucks promoting it (my little mini-conspiracy theory). Thanks for your contribution
You don’t need good science or vit. D or lower blood pressure. You need exercise. Sure a mostly vegitarian diet helps, and 100 mg of Vit D3 a day will prevent your next cold or flu. But if you are told you need statins, go take a long hike or better yet run as far away from that doctors office as possible. I suppose there may be rare individuals where exercise is not enough (I have never heard of it) but if you are anywhere near normal, If you run or jog 5 miles 4 days a week, heck even twice a week, you will not have hypertension. If you climb 100 flights of stairs twice a week you will not be able to remain overweight and high blood pressure will be your last worry. I like to run on grass, but not on pavement, so I chose stairs. I picked a ten floor building and I climb the ten floor ten times, up and down twice a week. And it is easy. Sure start with ten flights. Most anyone can do that. Then add a couple of flights each time. Twice a week and you will be fit and slender. Started this getting ready to climb to base camp Mt. Everest. I started in tennis shoes, then put on hicking boots, then added a back pack, then added beer to the back pack which we consumed in the process. And phooey on the two beers the doctors say – if you do run 5 miles or hike 100 flights a few times a week, you can handle a few extra beers and just about anything else you care to eat. Still I do avoid animal fats and fried foods but I eat most anything else.
A major part of the fun of doing these Doc Gumshoe pieces is seeing your varied & interesting comments, for which I thank you. A few comments in response:
Several of you mentioned inflammation, a complex & important topic, about which I can’t do more than make a passing comment. But let me tell you, it’s usually not inflammation itself that’s the problem. Inflammation is a response to some kind of pathology – the body fighting off infection, or attacking a foreign invader, or sending scavengers to carry off dead cells, or trying to repair tissue damage, or a host of other inflammatory reactions. And sometimes, as in autoimmune diseases, inflammation becomes chronic. I’ll put the whole topic in the queue for a future Doc Gumshoe.
I want to qualify what I said about treating high blood pressure by trying to restore basic health. I’m not saying that it’s impossible, and that therefore anyone with established hypertension is doomed to a lifetime drug treatment. But I am saying that as a rule, in the overall patient population, it doesn’t work. That may be because patients don’t stick with a rigorous life-style modification plan for a long enough period of time. And I don’t know how long that “long enough period of time” might be. And I don’t know what happens if, after the BP is brought down to normal levels through life-style modification, the highly-motivated person who achieves this goal slips back into the same old habits. But I can guess.
What I do know is that in most people hypertension doesn’t produce any symptoms, so the person who is under treatment doesn’t experience any improvement in symptoms and is not rewarded. That makes it difficult to stick with a plan that deprives people of a lot of things they really like.
On the other hand, those drugs – including hydrochlorothiazide, which several people mentioned – work pretty well. Yes indeed, every drug has side effects. But since the effort to treat high blood pressure in the US got into high gear, several of the consequences of high blood pressure – heart attacks, strokes, congestive heart failure – have decreased in incidence.
May I add here that I can’t agree with the point of view that established medicine, whether it’s the AMA or the FDA or any official body, is purely driven by the evil profit motive, whereas alternative treatments, whether holistic, natural supplements, acupuncture, homeopathy, have only the benefit of humankind at heart.
I took note of a number of other topics that you mentioned & will see what I can dig up about them. Vinegar? H2O2? Anatabine? I’m having a good time with this – it suits my curiosity & cussedness. Best to all, Michael Jorrin (aka Doc Gumshoe).
I had a heart valve repaired, but the others were also leaking, so I was tested for a heart transplant. I thought I would age out, 77 then, but they said I had young arteries and young veins. My kidneys knocked me off, they said I was within a week from needing regular dialysis. I was given a heart prescription which many people take, but for me, it took away my ability to breathe. I practice breathing all the time, whenever I think of it. I try to breathe in for 2 full seconds, out for 3. 2 years ago, I couldn’t do 1/2 second either way. But the body was also swollen and the heart wasn’t strong enough to slosh around the extra liquid. Every diuretic tried made me ill. Finally I applied freshmen chemistry, and figured out, if I can’t get rid of the sodium, don’t take it in. I cut down to 1000 mg/day, didn’t do it, then 750 mg/day, still terribly swollen, then 500 mg/day, and it started slowly coming down. I’m grateful that plain chocolate is low in sodium because candy bars are high. I can never have a slice of cake or cookie that someone else made, baking soda and baking powder are like pure salt. Can’t have store-bought bread either. I had to cut down on my favorite drink, no-fat milk, to 2 cups/day because of the sodium, I couldn’t afford 130 mg for each glass the way I drank it. I grumble with each 35 mg can of diet Pepsi, I’d rather have skim milk. I waste 1/2 hour soaking in a very hot tub alternate nights, but it’s all less time than real dialysis would take. Physically, I’m as I was more than 2 years ago, I can’t breathe when vertical so walking and standing are limited, I have terrible balance, and the same limited air is for standing or talking. My wonderful husband has put hand rails everywhere for me, and loves the no-sodium food I fix, but sometimes pigs out on potato chips or other salty snacks. My no sodium cakes are to die for, as are my pecan sticky buns. I want to go out and run and play. I used to walk 6 miles a day. Now I’m less active than a cement post. If I could breathe better, I’d probably live to be 100. I stay well oxygenated, there is a difference between not enough air to do things, not having air to give a 1-word answer if I’ve walked to the bathroom recently, and being sufficiently oxygenated. The latter I manage with daily practice. I don’t want tanks.
I tried anatabine for a full 1/2 year, before my heart surgery, didn’t help me, but then I’m so allergic to tobacco or tobacco smoke, that it bothers me to be close to someone who has a pack of cigarettes in his pocket. So it figures it wouldn’t help me.
Eat garlic!
Throughly enjoying your blogs, Michael. Can’t often agree, but am always amused, informed and interested.
A healthy amount of skepticism is a good thing. However, I have personally observed a close relation, who was given two weeks to live by board-certified medical specialists, and lived years longer due to judicious use of non-prescription supplements. As the saying goes “seeing is believing”, and I now believe that the vast majority of our US physicians are not properly educated on the medicinal use of non-prescription substances. That’s a shame, but also a reality, and nothing new. In the late 1940s, before the Salk vaccine, Duke University Medical School graduate Dr. Fred Klenner was curing polio cases with large doses of intravenous vitamin C. Somehow Dr Klenner’s tremendous accomplishments were never assimilated by mainstream medicine.
So my advice is to keep an open mind, and utilize both standard and alternative medicine to stay in good health.
Intravenous vitamin C has a long history of curing most any bacterial or viral infection but alas most medical doctors have never heard of it or discount it for lack of double blinded randomized trials. But it can’t be patented so no one will pay for such trials. Finding a doctor that will offer it is tough but I have read the testimony of some folks who have and recall one saying anytime she feels a cold coming on she gets the intravenous Vit. C and it is gone. Indeed mega vitamin C orally (and I recommend lots of Vit. D-3 with it) will often do the same thing. The catch is that we can’t tolerate too much oral Vit. C because too much produces loose bowels. When you are healthy and feeling fine that level might be 2000 mg of Vit. C. or less if you don’t take 1000 mg every day (as I try to). But the amazing thing is that when your body is fighting a pathogen like a cold or flu it can tolerate much more – it is as if the body knows or uses it up before it gives you the runs. I take one 1000mg timed release Vit C daily but any hint of a scratchy throat or sneezing and I start taking 5 or 6 or more a day for a few days and usually beat the cold off. I have heard this supported by both Dr. Julian Whitaker a well known MD who supports alternative therapies in his popular newsletter ‘Health & Healing” (and assails and discredits many of the normal medical treatments like statins for high blood pressure) , and by Dr. David Williams a DC who writes a similar popular newsletter “Alternatives” offering alternative therapies and at the same time discrediting select aspects of conventional medical care. Both, by the way, strongly support as highly effective for most any infection – even antibiotic resistant bacteria – high dose intravenous Vit. C.
I read about one remarkable case from New Zealand in which a patient was on life-support due to flu, and his family was advised to disconnect the life support. Instead they absolutely insisted on massive doses of intravenous vitamin C, and the given-up-for-dead patient walked out of the hospital several weeks later. My physician daughter advises me that so far only one patient is known to have survived rabies, and I can’t help but wonder if that fatal viral illness would also respond to massive doses of intravenous vitamin C. It seems there would be nothing to lose in trying.
After Linus Pauling asserted that mega-doses of vitamin C would cure just about anything, there was a lot of close scrutiny on it’s efficacy. Unfortunately, about 15 clinical studies came up motly empty. Currently, 60 clinical studies are being conducted on Vitamin C in cancer, including prostate, pancreatic, colorectal, liver, multiple myeloma, non-Hodgkins lymphoma, uterine cancers, includng in patients who have not responded to all other current treatment. Many of these trials are being done in academic centers, for example, the University of Kansas is studying intravenous vitamin C in cancer. Pub Med lists 1794 published papers that discuss cancer and Vitamin C. The fact that Big Pharma does not stand to make a lot of money from Vitamin C doesn’t stop the research. I personally pop a Vitamin C when I feel a cold coming on, and maybe I’m fooling myself, but it seems to help. At least it doesn’t hurt, as far as I can tell. The Vitamain C story is not finished.
Vitamin C isn’t known to cure cancer, but IP6 (Inositol hexaphosphate) just possibly might. Anyone who is concerned about cancer might wish to read a book by Professor AbulKalam Shamsuddin MD PHD (U Maryland Medical School), or else start with this free ebook by two of his admirers:
http://www.inocell.com/pdf/toogoodtobetrue.pdf
As Dr Shamsuddin writes, the government stopped researching IP6 after calling it “highly promising” because it didn’t fit their experimental protocol for chemotherapy: large oral doses instead of small intravenous doses , non-toxic instead of toxic, etc.
Best of health to everyone!