[ed. note: Michael Jorrin, who I call “Doc Gumshoe,” writes for us a couple times a month on health and medical issues — he is a longtime medical writer (not a doctor), he chooses his own topics, and his past articles can be found here.]
Flub Number One is the puncture of the “female Viagra” hot-air balloon, to which I say, “So be it!”
Flub Number Two is the failure of Eli Lilly’s evacetrapib, one of a new class of drugs to treat hyperlipidemia, on which high hopes were riding. To that unfortunate outcome I say, “Too bad, but what can we learn from it?”
And the Big Question Mark has to do with CRISPR gene editing, a topic that has many scientific brains quivering with excitement. My question, which I will explore in this piece, is “What will that actually mean for health care?”
So, on to the first flub. On August 18th, 2015, the FDA disregarded my careful and intelligent advice, which I had set forth in my Doc Gumshoe blog on July 2nd, and approved flibanserin, the so-called “female Viagra,” which was trade-named Addyi. My reasons for opposing the approval were, as I said then …
“I think FDA approval of this drug would do more harm than good, and I hope the FDA resists the pressure that is being placed on it and rejects the application.
The drug is flibanserin, which was initially developed by Boeringer Ingelheim, who dropped it after the FDA rejected it twice – first in 2010 and then again in 2013. A very small company, Sprout Pharmaceuticals, then acquired the rights to flibanserin. Since then, Sprout has mounted a campaign to persuade the FDA that flibanserin should be approved based more on the “fairness” issue than on efficacy and safety.
The “fairness” issue can be stated simply, although somewhat moronically in my view: There are a couple of dozen drugs approved by the FDA that improve sexual performance in men, but there are no FDA drugs that do the same for women. That constitutes gender discrimination. Therefore flibanserin must get FDA approval, regardless of its efficacy and safety data.
Sprout has organized and backed a pressure group called “Even the Score” whose mission has been to mount a campaign whose theme is that the lack of a drug that improves women’s sexual desire is a glaring example of the FDA’s gender bias. And, of course, the phrase “Viagra for women” is the slogan that sums it up.”
Well, the FDA went ahead and approved it anyway. But their approval was more than a bit tentative. Here’s part of the warning label in the patient PI:
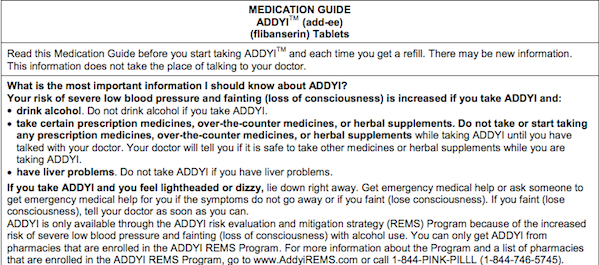
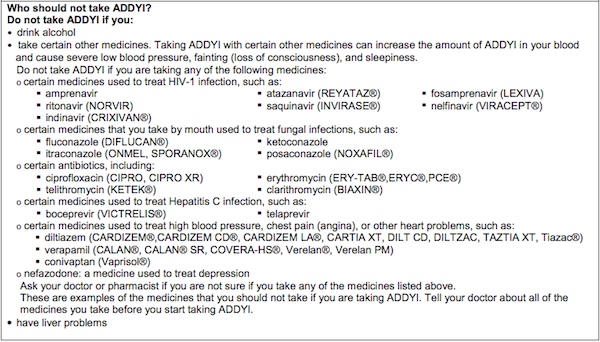
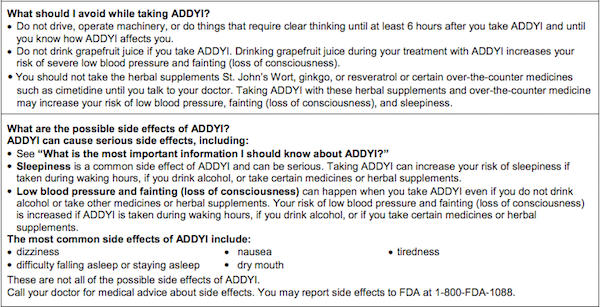
The FDA was perhaps making a show of giving in to Sprout’s propaganda campaign, but the patient PI looks to me like the “bacio di morte,” although the immediate outcome for Sprout was far from fatal. A day after the FDA’s approval of Addyi, Sprout Pharmaceuticals was purchased by none other than Valeant Pharmaceuticals International (VRX) for One Billion U. S. Dollars. Sprout took the loot to the bank, and thereafter grief was visited upon Valeant.
Valeant’s first step was to double Sprout’s proposed $400 per month charge for the magic pills to $800 per month, as per their usual practice. Since then, Valeant’s stock has fallen about 85%, President J. Michael Pearson is out, and his couple of billions in stock is worth bubkas. Only 4000 prescriptions for Addyi were filled in the six months after FDA approval. It’s not hard to figure out why. The benefits in terms of improvement in sexual satisfaction are very small, the limitations on life-style are considerable, and the risks are truly serious. Valeant should have paid attention to the data, but that’s not their strong suit.
The diminished promise of CETP inhibitors
It’s no doubt quite unfair to refer to the failure of the evacetrapib clinical trial as a “flub.” Evacetrapib was one of Eli Lilly’s (LLY) top prospects, and with good reason. It further lowered LDL-cholesterol (LDL-C) in persons who had already attained good LDL-C levels with statin treatment, and, in addition, it more than doubled HDL-cholesterol (HL-C) levels, which statin treatment only affects minimally. The failure of that trial was a surprise and disappointment to the cardiovascular community. Dr Peter Libby, who is about as famous as cardiologists get, was quoted in the Times as saying “All of us would have put money on it. It was the great hope.”
The evidence that lowering LDL-C leads to a reduction in cardiovascular events is about as good as this type of evidence gets: a reduction of about 40 mg/dL in LDL-C reliably lowers the risk of an acute coronary event by about 20%. Depending on baseline levels, high-dose statin treatment can lower LDL-C levels by 50% or more, with concomitant reductions in cardiac risk. However, with statin treatment, LDL-C levels seldom go much below about 70 mg/dL, and cardiac risk does not disappear.
Many clinicians have sought to further reduce cardiovascular risk by adopting strategies to increase the levels of HDL-C through some other means, such as fibrates and nicotinic acid, both of which are severely limited by adverse effects. The association of a beneficial role of high-density lipoprotein (HDL) with reduced incidence of cardiovascular disease (CVD) is almost as strong as that for LDL-C and CVD, although more recent. The standard explanation for this relationship is that the HDL particles are the key players in reverse cholesterol transport, meaning that they gather up cholesterol in the circulation from low-density-lipoprotein (LDL) particles, and transport them back to the liver for elimination.
At the risk of going over old ground, I want to be clear about the terminology used to describe cholesterol and cholesterol transport. Low-density lipoprotein (LDL) is not the same as the cholesterol transported by low-density lipoprotein, which I scrupulously designate as LDL-C. Same thing with high-density lipoprotein (HDL) and high-density lipoprotein cholesterol (HDL-C).
Recent findings about cholesterol metabolism and transport muddy the waters considerably. Although the observation certainly holds true that higher levels of HDL-C relative to LDL-C are linked with better cardiac health, the mechanisms that affect the formation of HDL-C are highly complex, and it is not clear that introducing agents that affect these mechanisms will have a predictable outcome.
The two players in overall cholesterol metabolism that are central to the potential effectiveness of CETP inhibitors are cholesteryl ester and cholesteryl ester transfer protein (CETP). Cholesteryl ester is a molecule consisting of cholesterol chemically bonded to a fatty acid. (This is different from LDL-C and HDL-C, where there is no chemical bond between the cholesterol and the lipoprotein.) The cholesteryl ester molecule can be split back into cholesterol and the fatty acid by an enzyme. In the liver, cholesteryl ester is transported by CETP, conveying cholesterol between any of several lipoprotein particles, including from HDL to very low-density lipoprotein (VLDL) and LDL, as well as between HDL particles of different sizes. So it would seem intuitively reasonable that if a way could be found to prevent this CETP from moving the cholesteryl ester (which contains cholesterol) out of HDL and into the atherogenic VLDL or LDL particles, that would lead to higher HDL-C levels, which would be a good thing.
Four different CETP inhibitors have been developed with this objective, and have progressed to advanced clinical trials. All four have somewhat different mechanisms of action, which no doubt account for the considerable variation between the results of these trials. Torcetrapib, from Pfizer (PFE), was scrapped after a trial in which subjects taking the drug experienced significant increases – increases, not decreases, as expected – in cardiovascular events and mortality. Dalcetrabib, from Roche (RHHBY), produced much smaller increases in HDL-C, and has been sidelined as ineffective.
Eli Lilly announced in October of 2015 that they were discontinuing development of their CETP inhibitor, evacetrapib. At the American College of Cardiology meeting in April 2016, they explained why. In spite of excellent clinical trial results in terms of increasing HDL-C (by 130%) and lowering LDL-C (by 37%), no benefit whatever in terms of health outcomes was conferred on the subjects in the trial. The trial, ACCELERATE, enrolled more than 12,000 subjects, all of whom had established cardiovascular disease, and about half of whom were on concomitant statin therapy. During the trial, 92 patients taking evacetrapib sustained strokes, compared with 95 patients taking placebo. And 434 subjects taking evacetrapib died from an acute coronary event, compared with 444 subjects taking placebo.
Anacetrapib, from Merck (MRK), may be the last CETP inhibitor standing. Given in conjunction with statins, it produces a large increase in HDL-C of about 140%, without adverse cardiovascular side effects. Currently, a large trial in anacetrapib is under way (about 30,000 subjects), with results expected in 2017. Expectations are not all that high, having been dimmed by the evacetrapib failure. But the anacetrapib trial is larger, and the subjects in the trial are somewhat different, so there is a hope that the increase in HDL-C, which is very similar to the increase produced by evacetrapib, will have significantly different results in terms of benefits.
"reveal" emails? If not,
just click here...
In the meantime, what conclusions – if any at all! – might be drawn from the evacetrapib bust? One, surely, is that surrogate endpoints have to be viewed with a degree of skepticism. This has always been a Doc Gumshoe principle, and it appears to be borne out in this case. Employing surrogate endpoints (the easily measureable HDL-C and LDL-C levels) in clinical trials is essential; researchers would have to wait a really, really long time if only hard endpoints such as death or signal events were used. And at the same time we need to remember, for example, that it took 90 years to demonstrate that lowering cholesterol actually resulted in a benefit in terms of reduced cardiovascular risk. Statins worked, eventually, while a low cholesterol diet did not work. The “how” mattered as much as the “what.” In the particular case of increasing HDL-C levels, it appears to matter just what means are employed to accomplish this increase. CETP inhibitors affect a complex system, and it appears that the results are not easily predictable.
A second more tentative conclusion is that there will be a renewed focus on the anti-inflammatory properties of statins, which are known to affect the levels of nitric oxide by a variety of means – nitric oxide being involved in anti-inflammatory activities.
Finally, it seems likely that the territory of cholesterol-lowering beyond that attainable with statins may be left, at least for now, to the PCSK9 inhibitors, which we have written about several times (April 2014, for example). PCSK9 inhibitors are hugely more expensive than statins, and my guess is that the use of these agents will mostly be limited to patients with familial hypercholesterolemia and patients who cannot tolerate statins due to adverse effects. But statins have a bad reputation in some quarters, and PCSK9s will no doubt get cheaper over time, so we’ll keep watching.
At the same time, I’m pretty sure that research will continue into the CETP mechanism and the possible benefit of agents that in some way affect that mechanism. Whether or not a useful agent comes from that research is anybody’s guess, but the subject is way too interesting to be abandoned just because several Big Pharma outfits have poured billions down the drain investigating it, with no results so far.
Where will CRISPR-Cas9 gene editing lead?
I’ll try to elucidate that strange acronym a bit further on in this piece, but let me kick it off by stating, without fear of contradiction, that gene editing is a reality. Scientists can dispatch this nifty new device (we’ll call it a device, for now) to a precise target on the genome of a plant or animal, and snip out a little piece of it. They can also substitute a different bit of genetic material for the bit they snipped out. The genome of that plant or animal is now fundamentally different, and descendants of that plant or animal will now carry that genome, with all the characteristics that it determines, from that time forward. It is an enticing and at the same time rather scary prospect.
Deleting genes is definitely less controversial than altering the genome by inserting a different gene. Many crops which are subject to specific genetically-determined shortcomings may be able to be improved by removing the culprit gene or genes. Scientists have already developed an experimental strain of wheat that will likely be completely resistant to powdery mildew, a disease that annually causes huge damage to wheat crops, reducing yields by as much as 15% in some regions. Susceptibility to powdery mildew is genetically determined by three genes that reside at different locations on the genome. Using the CRISPR-Cas9 cluster of DNA sequences, the powdery mildew genes were cut out of the genome. It should now be possible to propagate that resistant wheat species, and, in time, grow wheat crops that will not be affected by powdery mildew.
A highly important feature of this technique is that it avoids the GMO pitfall. The resistant wheat strain created in this way is not a genetically-modified organism in that it does not carry any foreign genes. Its genome is entirely its own, the only change being the extirpation of the sequences that make it susceptible to the powdery mildew disease. I am by no means in the camp of those staunchly opposed to anything GMO. Nature has been introducing “foreign genes” into the genomes of plant and animal species since year dot and will no doubt continue to do so, sometimes with beneficial results, and sometimes not. My concern with GMOs is mostly that I do not want to see single genetic varieties becoming dominant. There was a time when the only kinds of apples you could buy were Red Delicious and Macintosh, not because they were GMOs, but because they had been hybridized and found to be popular. Happily, that time has passed. Biodiversity has triumphed, at least in the apple department, and so it should in every other department.
An example of potentially fatal consequences of the absence of biodiversity was the Irish Potato Famine, which occurred around 1850 and resulted in about one million deaths. An important cause was that one potato variety, the so-called Irish Lumper, accounted for the principal nourishment of about two-thirds of the population at that time. It was a very large, easy to grow spud that needed hardly any cultivation, and when the potato blight (Phytophthora infestans) attacked, there were no alternative potatoes and little else for nourishment. Therefore, people starved. However, even if a powdery mildew-resistant wheat variety becomes dominant, there is minuscule danger of a similar disaster striking, since there are seed banks with all manner of alternative seeds of every imaginable crop.
When it comes to gene editing as a means of addressing diseases in humans, the potential is unquestionably there. Obvious examples are diseases that are determined by a single defective gene, such as Huntington’s disease (formerly known as Huntington’s chorea, because of the jerky writhing movements that patients demonstrate as the disease progresses). A child who inherits one copy of that gene has a 50% chance of developing the disease, for which, at present, there is no cure. The folksinger Woody Guthrie was diagnosed with Huntington’s chorea in 1952 and lived with it, in increasing distress, for about 15 years until his death in 1967. Woody’s children, including Arlo Guthrie, have evaded the curse.
It is likely that at some point in the not-too-distant future, the defective gene may be able to be removed in embryos when a parent has the defective Huntington’s gene, removing the risk for that individual. The offspring of the adult human that develops from that embryo would similarly be immune from Huntington’s disease. That goes for any gene that determines a specific disease. However, in most diseases that have a genetic component, many different genes located in different parts of the genome are factors in the disease. It would be much, much more difficult to address the disease if it required wholesale tinkering with the genome.
Another factor that needs to be considered is, what else does that gene do? Take the gene that causes sickle-cell anemia, a genetic disease which is more common in Africa and in persons of African descent. Sickle-cell anemia is due to a mutation in the gene that encodes hemoglobin, which is the blood component that transports oxygen, and only individuals that inherit two copies of the gene develop the disease. Since sickle-cell anemia significantly shortens a person’s life span, it would stand to reason that inheriting two copies of this mutated gene would be exceedingly rare. However, paradoxically, in some regions as many as 40% of the population carry this mutation. Why could this be? Well, it turns out that persons carrying just one copy of the mutated gene, who do not develop the sickle-cell disease, have inherited a huge benefit: they are largely immune from malaria, so the single copy of the sickle-cell gene is a vital protection against a disease that kills millions. Do we want to attempt to cure sickle-cell anemia by editing out the mutated gene by means of CRISPR-Cas9? I don’t think so.
CRISPR is a group of RNA sequences whose components – adenine, guanine, cytosine, and thymine – read the same forward or backwards. The name stands for “clustered regularly interspaced palindromic repeats.” Cas9 stands for “CRISPR associated protein 9.” CRISPR has the capacity of precisely recognizing specific sections of the genome, and Cas9 is an enzyme that cleaves the DNA strand at that specific spot. CRISPR-Cas9 can also insert a DNA sequence into a genome. The CRISPR-Cas9 grouping was discovered in bacteria, which employ this device to protect themselves from viruses by finding and inactivating target sequences in the viral DNA. CRISPR-Cas9 can be inserted into the class of cells that are passed on from one generation to the next, the so-called “germline cells,” and so genetic modifications inserted into the genome of the parent would be passed on to the next generation, and the next, and the next.
The community of molecular biologists is rightly concerned about the implications of CRISPR-Cas9 for gene editing in humans. One widely publicized experiment in human gene editing was done in China, on 86 human embryos that had a gene that would result in a rare but fatal blood disorder, beta thalassemia. These embryos had, in addition to the blood disorder, a fairly common defect that would prevent them from developing into viable babies, so there was zero likelihood that the gene editing experiment would have results in human beings. The researchers attempted to swap a normal gene for the defective beta thalassemia gene, with signal absence of success; most embryos did not retain the DNA that they had attempted to insert. The CRISPR-Cas9 device also, apparently, made a number of unintended or erroneous edits. What this experiment did was indicate clearly that the prospects for gene editing in humans are far in the future – if ever.
Many of the most prominent among the researchers in this field have called for a moratorium on gene editing in humans, but the prospects for employing this technique for other purposes continue to be lively. One specific project, now being pursued at the Harvard Chan School of Public Health, seeks to genetically engineer mosquitoes so that they will not transmit Plasmodium falciparum, the micro-organism that infects humans with malaria. Accomplishing this feat in such a way that the particular anti P. falciparum trait gets transmitted throughout the entire Anopheles gambiæ population would have immense beneficial consequences for us humans. Something like 200 million people get malaria each year, and this results in about 600,000 deaths. We, in developed nations and temperate climates, do not worry much about malaria, but about half of the world’s population lives in regions where malaria is a constant threat. People who travel to those regions are generally advised to take careful precautions against being bitten by mosquitoes, and also to take anti-malarial drugs, such as chloroquine. You may remember from your youthful reading of adventure stories set in exotic locales that the heroes and heroines were always dosing themselves with quinine – as well as drinking gin and tonics, made, of course, with quinine water.
The threat of malaria would likely end, once and for all, if those mosquitoes would simply stop transmitting the malaria parasite. Not just some mosquitoes – all the mosquitoes that currently transmit P. falciparum. Is this conceivably even feasible? As it happens, some mosquitoes already have a genetic trait that essentially prevents them from transmitting malaria. They can bite a person with malaria, and then, when they get hungry again and want another blood meal, they find another victim to bite, but they don’t give this next victim malaria. They have a sort of genetic immunity to P. falciparum.
Researchers are working on an ambitious project: isolate the genetic sequence that made those mosquitoes into non-malaria transmitters, and insert that gene into the DNA of female mosquitoes, whose offspring would then also be non-malaria transmitters. But in order to make sure that those offspring would indeed carry the female mosquitoes’ genes, rather than the genes of the wild male mosquitoes, another step would be necessary. Some genes in nature appear to be equipped with tools that make them into dominant genes. Researchers call this “the gene drive.” The genes have a sort of tool kit that lets them spot a genetic sequence, remove it, and replace it with their own genetic sequence. So a similar gene drive would have to be inserted into the DNA of those female mosquitoes, to make sure that the genetic immunity to P. falciparum would be passed on to future generations in every single case.
The next step would be to breed, in the laboratory, a huge swarm of these non-malaria transmitting females, and then release them into the wild where they and their offspring would replace the current population of malaria transmitters. No one is underestimating the enormous scope of this proposal. For one thing, mosquitoes do not seem especially eager to reproduce in the laboratory. Something about those sterile surroundings seems to dampen their erotic inclinations. But even more important, the areas of our planet where malaria is a threat are vast. They include most of sub-Saharan Africa and large parts of Asia and South America. There would have to be many, many mosquito releases in many, many areas, especially because mosquitoes do not travel long distances from the places where they hatch – seldom more than a few hundred yards. One good thing is that mosquito reproductive cycles are very short, so there could be several generations of mosquitoes hatching out and reproducing during the course of a single year, and if all those new mosquitoes were transmitting the anti-malaria gene, that gene would indeed spread. But the task of breeding and releasing those mosquitoes would be colossal.
A similar proposal for controlling the Zika virus would entail creating immense numbers of sterile Aedes aegypti males – not females – and releasing them into areas where Zika is prevalent. Presumably, those sterile males would mate with females and produce no offspring. Female mosquitoes are highly moral little creatures (except for their unfortunate tendency to bite people) and they only mate once in life, so having succumbed to the attractions of the sterile male, they have lost forever their chance to reproduce their species. I cannot see that as a promising route to the elimination of the Aedes species, unless, somehow, those sterile males were vastly more sexually attractive than their still fertile brothers, of which there would continue to be lots and lots. An exceedingly long shot, I call it.
Despite the habitual Doc Gumshoe skepticism with which I view scientific developments that are the subjects of full-bore PR campaigns, I do think that CRISPR-Cas9 gene editing is a highly promising field of investigation. As some of you may have learned, there are patent squabbles going on, suggesting that there may be big money payouts resulting from research in this field. Jennifer Doudna at UC Berkeley and Emmanuelle Charpentier at the Helmholtz Centre in Germany got the first patent, in 2012, and Feng Zhang at Harvard’s Broad Institute, and George Church, also of Harvard, demonstrated in 2013 that CRISPR could be used to edit human DNA, and Zhang was awarded a patent on that technique.
One more example: it would be theoretically possible to prevent HIV by means of gene editing. A variant of the CCR5 protein has been found to block the entry of HIV into human cells. If this variant were introduced into the human genome, it could very significantly prevent the spread of AIDS. However, this variant, the Δ32 mutation, would increase our susceptibility to West Nile virus. Is that a risk worth taking? That’s the kind of question that the proponents of CRISPR-Cas9 will continue to be faced with: if they tinker with any part of the human genome, supposedly in order to achieve benefits, what other possible consequences might that have? Those questions need to be addressed and answered scrupulously and painstakingly in every single case.
* * * * * * *
I’ve taken note of some questions about specific new and experimental drugs that readers have spotted and will try to come up with something useful. And Travis has told me that several of the Gumshoe faithful have asked about miracle cures that have perhaps a “miraculous” provenance, namely, Holy Writ. I’m working on it. Best to all, Michael Jorrin (aka Doc Gumshoe).
Very good article. I’m very interested in the CRISPR/CaS9 stuff and plan to cover it going forward. I’ve already put two notes out (links below) and am keen to do more. These two (EDIT and NTLA) are the first two big public companies on the CC9 bandwagon and I expect more. The science is fascinating and the potential seems huge but it feels like an area that will be subject to all kinds of hype and misunderstanding. Keep the great articles coming! Love it!
https://ipocandy.com/2016/02/a-crispr-view-of-editas/
https://ipocandy.com/2016/05/intellia-ntla-jumps-crispr-ipo-bandwagon/
In China, they are experimenting with HIV prevention in the foetus, at Stanford, they have produced rats that got younger—the push towards human immortality will drive this (and other) procedures onto human use. Legislation is needed NOW, before the procedure explodes beyond any ability to control it.
thanks Gum…. I went through it, will have to go a few more times to get the info correct!… Highly technical, and highly informative.
many many thanks, and also for the other techie things you do so well!
THANKS FOR BEING YOU
Great read! Thanks for the overview.
Several things you said caught my eye.
“The community of molecular biologists is rightly concerned about the implications of CRISPR-Cas9 for gene editing in humans.” Considering that “we are what we eat” then it seems logical that these biologists should also be rightly concerned about the implications for gene editing of our food supply. The power of this technology, and the potential for something to go wrong should not be underestimated where it concerns our source of nourishment either.
“Another factor that needs to be considered is, what else does that gene do?” Because the CRISPR-Cas9 technology is essentially a more precise means of gene manipulation than previous techniques does not necessarily eliminate unintended and unanticipated consequences. It’s OK if the consequences are recognized before release into the environment, but our current regulatory system has proven to be utterly unconcerned about requiring long term studies to determine long term consequences. In fact, it is a total fallacy that the FDA does independent studies. They rely completely on corporations to supply their own safety testing data AND THE PROTOCOL. Currently the default time period of testing is a mere 3 months whereas independent researchers have called for 2-year studies as a minimum.
“That’s the kind of question that the proponents of CRISPR-Cas9 will continue to be faced with: if they tinker with any part of the human genome, supposedly in order to achieve benefits, what other possible consequences might that have? Those questions need to be addressed and answered scrupulously and painstakingly in every single case.” I hope others see your point as well. However, the FDA and USDA currently are bending over backwards to accommodate whatever new genetic manipulations are offered for approval, with NO long term studies to establish safety. This is in spite of the original strong concerns and recommendations for long term studies expressed by many of the scientists at the FDA when looking at the new technology of gene manipulation in the 1980’s, as revealed in Freedom of Information Act documents obtained from the FDA. While corporations have managed to enact legislation granting specific legal immunity for any consequences due to their manipulated products, there is a lot of growing concern among primary care doctors who see a risign tide of chronic and acute diseases across the population that hasn’t been adequately explained, but the food supply is a strong contender as the culprit simply because everybody eats these foods.
Making genetically modified bacteria that can convert CO₂ into cleaner jet fuel and fighting zica and malaria with genetically manipulated mosquitoes may work well or may not, it’s worth a try, but it isn’t the same direct impact on humans as fiddling with what we eat to nourish our bodies. That wheat, and all other biotech derived foods should be held to a much higher standard of testing than they will actually get. Because they are not, I won’t invest in them, I don’t want the bad karma if people get hurt, nor the losses if the rest of the world won’t accept it. The biotech food industry is starting to falter and reel under the backlash already, and the vast majority of their products are solely for the purpose of making crops resistant to more and more toxic chemicals. It’s not sustainable. I won’t touch it.
And I won’ eat it….and don’t think it’s too much to ask just to label it.
Unfortunately it will still continue and in some ways may be unstoppable from here on. You have my vote.
Thank you for this valuable article. For 2 decades I have followed genetic modification (with and without viral foreign proteins inserted), RNA enzyme and protein production like Sanofi’s (pharmaceutical path which derive from petrochemicals leaving intermediates and metabolites which build up in the cells or yeast origins which do not) and stem cell therapies. I do not understand why with the inborn errors of metabolism we have not (to my knowledge) tried to correct the known genetic deletions by inserting the healthy protein/enzyme production back into the DNA instead of just inserting for that organism at the RNA level (or trying to make new healthy cells from stems). I have owned EDIT almost since it became available and would appreciate your insight on that patent capable finding of the lady doctors.
CB MD: Have you thought about joining the Irregulars? With your background you should be easily able to put your 2c worth in the cerebral discussions there. Dr KSS would no doubt know why RNA and not DNA is the target.
Regards,
Penny
There is actually an effective remedy for treating Women’s sexual dysfunction. Our team has formulated with success, a therapeutic method that is effective in 98% of Women. It is actually an easy solution with the medication that we have discovered. Please contact us at the above email. Thank you for your article and continued educational material. Very interesting reading material, but you may find our solution to Women’s sexual dysfunction fascinating.
Which email above?
Alan, his username is a hyper link, so I think that’s where you’ll find it.
$ORMP
Anyone familiar with Israeli Oramed Pharmaceutical Co that is testing an oral insulin treatment mainly for Type II diabetics?
Here is the news release: http://www.oramed.com/category/press-releases/
From a Reuters article: “While insulin is typically associated with type 1 diabetes, many patients with type 2 eventually see their disease progress to the point where they need insulin. Type 2 accounts for more than 90 percent of the nearly 400 million people with diabetes worldwide.
A safe and effective oral insulin, if approved, is expected to become a multibillion-dollar product.
The main attraction of an insulin pill, aside from avoiding injections, is that it comes much closer to the path of natural insulin, which is produced in the pancreas and goes directly to the liver. ORMD-0801 goes from the gut to the liver, while injected insulin circulates throughout the body before it gets there.
Some doctors believe high levels of insulin circulating through the rest of the body may increase health risks. “
I am. It’s junk.
Also, the distinction between oral and therefore liver-first-pass insulin and systemic insulin is functionally specious….it’s PR BS from the company.
Thanks.
The failure of Lilly’s CETPi paves the way for unparalleled success with ATP citrate lyase inhibitor bempedoic acid from Esperion ($ESPR) to become the preferred first-line lipid mgmt drug.
Long $ESPR.
Sorry for not answering comments sooner. The outfit that markets the treatment for enhancing female sexuality is Synergistic Therapeutics. The product is applied externally, guess where. No hint on their website what the active ingredients might be. The mere act of applying it externally might have some effect. As for oral vs injected insulin, I’m with Dr KSS. Remember that we need to metabolize glucose in every town & village in our bodies, so we need insulin everywhere. Re Esperion’s candidate, it will still have to slug it out with statins, which have a colossal economic advantage. And while I do favor labeling GMOs & would favor similarly labeling food products genetically modified by means of gene tinkering, I mostly aint’ scared of them. What is cross-breeding but genetic manipulation? Have you tasted the new “breed” of blackberries lately? They’re yummy! Best to all, MJ
Externally where? Are they talking an “external” version of Spanish fly? The mind boggles.
“…the lack of a drug that improves women’s sexual desire is…gender bias…”
Totally specious argument, based on the myth that Viagra is an aphrodisiac – that it increases “desire”. It does nothing of the sort: it allows performance by enabling erection.
So? Now they are marketing a drug for female erection?
Doc:
Likes many others, I’d like to thank you for writing. The clarity of your writing, even with the complexity of the material, is a joy to read. Between your contributions and those of Dr KSS, I feel much better informed. I share your opinion on GMO and hybridizing too: that approach just seems sensible, though I’m a bit skeptical about hybridizing.
In that regard, awhile ago Prevention published a book about the evils of wheat, specifically induced by recently introduced hybrid versions. The author advised aggressively avoiding wheat and related products (e.g. some soy sauces0, suggesting doing so would lead to better health. Do you have any observations on that line of reasoning?
Thanks for the article.
But you forgot the word “short” when you listed the words in the CRISPR acronym. It should be: “clustered regularly interspaced short palindromic repeats.”
Thanks to all! Yes, I left out “short” – and the CRISPR sequence has to be relatively short to function. Re the “female Viagra” nonsense, what Rusty Brown in Canada said is more or less what I said in my original piece. Viagra enables erections and is taken specifically when the male wants to have sex. Addyi theoretically turns up the dial on the female;s underlying desire for sex, and must be taken chronically, and even at that doesn’t work very well. The proposed new treatment supposedly contributes to female sexual arousal, who knows how, or with what other possible consequences. As for red flags about wheat, it’s harmful to about 1.3% of the population, i.e., people with celiac disease. It has a high glycemic index, particularly when refined, and could contribute to type 2 diabetes. But billions of people rely on it, and I see no evidence that non-wheat eating populations have better health outcomes than wheat eaters, which include all the developed countries. It’s perhaps possible tp craft a diet that includes no wheat or wheat products, and it might – or might not – lead to better health in some individuals, but I can’t see it being practical for the multitudes. Best to all, MJ