These days, if you ask people what diseases they are most concerned about, you’ll likely get a pretty wide range of answers. In spite of the tapering down of the pandemic, some people will certainly pick COVID 19 as their bugaboo. But there are lots of competitors for the top spot on the list. Flu is gaining ground in this nasty contest, and monkeypox is still around and causing suffering, although mostly in a limited population. People with young children are rightfully worried about respiratory syncytial virus (RSV), which is slated to be of considerable concern this season. Alzheimer’s scares us as we get older, and cancer is undeniably a menace. And individuals have individual concerns, relating to their own risk factors and pre-existing conditions.
What I don’t see as a disease that lots of people are fretting about is heart disease, or, if you prefer a broader classification, cardiovascular disease. Just about everybody acknowledges cardiovascular disease (CVD) as a threatening presence, but we seem to accept it with a shrug, as part of that all-encompassing “something” that is bound to get us.
But in fact, cardiovascular disease is the leading cause of death here in the US and also here on Planet Earth. In the US in 2020, 697,000 people died from CVD – that’s one death every 34 seconds. CVD was the cause of approximately one fifth of all deaths in the US before the onset of the COVID pandemic. The percentage varied between males and females, with males experiencing a somewhat higher percentage of heart disease fatalities, and also between ethnic groups. Non-Hispanic whites had the highest percentage of CVD fatalities – a bit over 21%, closely followed by non-Hispanic blacks. The lowest percentages, around 14%, were in American Indians and Alaska natives.
(I should point out that the likely difference between ethnic groups is not that one group is intrinsically healthier than another – Alaska native individuals are not healthier than non-Hispanic whites. Rather, it’s that they perished owing to other causes than cardiovascular disease.)
Globally, before the COVID pandemic struck, almost 18 million people died every year of a cardiovascular disease, and this accounted for about 32% of all deaths on the planet. About 85% of those deaths were due to heart attacks or strokes.
At least three-quarters of CVD fatalities happen in lower-income parts of the world, and many of these deaths can be attributed to behavioral factors including tobacco use, poor nutritional conditions, obesity, and other modifiable factors. Of course, those factors are also present in the upper-income regions, but in those regions efforts to modify those conditions have begun to have an effect. For example, more than 80% of smokers live in low-to-middle-income countries. China is the world’s leading smoking country, producing and consuming almost a third of the total number of cigarettes on the planet. In China, 74% of the men are smokers, but only 8% of the women smoke. In the US, smoking prevalence dropped from 42% of adults in 1965 to about 14% in 2018, which is reflected in greatly reduced CVD mortality rates.
Which means that there is some good news about cardiovascular disease mortality in contrast with those grim statistics. In the more developed parts of the world, CVD mortality has declined. For example, if heart disease rates in the US had remained at their 1996 peak, there would have been about 10 million more deaths attributable to heart disease since that date. There has also been a huge decline in stroke mortality, from nearly 90 per 100,000 population in 1950 to 36 per 100,000 overall in 2018. Stroke mortality was higher in non-Hispanic blacks, at 52 per 100,000, but still much lower than it had been as recently as the year 2000.
Since 1990, the global mortality rate for CVD, standardized for age brackets, has declined by 27.3%. That decline has mostly been seen in the more developed parts of the world. However, because global population has increased, the total number of deaths has increased by 42.4%.
The general decline in CVD mortality is partly due to widespread improvements in treatment, and particularly in the availability of treatment. In the developed world (at least!) a great many persons are being treated for high blood pressure and elevated cholesterol, and also for the diseases that contribute to CVD, such as diabetes. Most of those treatments have been around for several decades, and some advances in treatment have emerged more recently. Doc Gumshoe is not going to get into those in this discussion. I’ll save it for another installment.
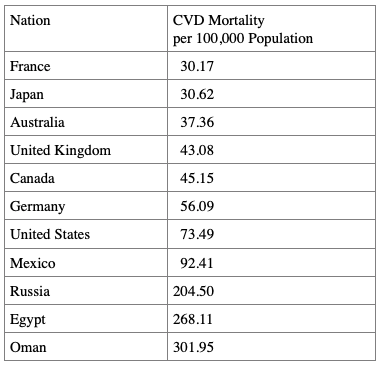
Here’s a greatly abbreviated table of death rates from CVD per 100,000 population, culled from the much larger table from the World Health Organization, mostly to emphasize the differences in mortality rates in different parts of the world.
These differences are certainly not due to differences in the disease itself, but to profound differences in such matters as availability of health care and prevalence of aggravating factors such as smoking. The mortality rate in the US is more than twice as high as the mortality rate in France, perhaps because France has a health care system that is available to all residents of the nation. I included Egypt and Oman as examples of the very high mortality rate in less developed parts of the world. And Oman is far from being the nation with the highest mortality rate – that dubious honor belongs to Tajikistan, with a mortality rate of 389.75, about twelve times the mortality rate in France.
I need to insert an unfortunate reminder here. If CVD causes 32% of deaths on the planet, the other 68% of deaths must be due to some other causes. And if in general, the percentage of deaths caused by CVD is declining, then deaths from other causes must be increasing. What might those causes be?
One of the direct results of that reduction in the CVD death rate is that – at least in those parts of the world where that death rate is indeed declining – the population is aging, and that aging population is susceptible to a number of other diseases especially associated with aging. So, as we’re spared heart disease, we are at higher risk of cancer, Alzheimer’s disease, Parkinson’s, and other such plagues.
Cardiovascular disease is fundamentally different from those other major killer diseases. It is not caused by infections, whether from bacteria or viruses. It is not caused by the mutation of our own cells, as in cancers. In the great majority of cases, CVD is caused by modifiable lifestyle factors, such as obesity, lack of physical activity, hypertension, an unhealthy diet, cigarette smoking, and excessive alcohol consumption. Comorbidities such as diabetes also contribute to the development of CVD, primarily through the harmful effects of diabetes on the circulatory system.
The American Heart Association recently (18 August 2022) published a review of the six principal cardiovascular disease entities, describing the main symptoms of each CVD. The review details the most reported symptoms of six cardiovascular diseases: heart attack, heart failure, valve disease, stroke, heart rhythm disorders, and peripheral artery and vein disease. It notes that there are important differences in symptoms between men and women, and points out that depression, which is common in many CVDs, hampers the individual’s ability to detect changes in his/her symptoms. Thus, effective methods of monitoring and measuring symptoms over time are essential in the management of CVD and in the effort to prevent or delay its progression. The AHA review emphasized symptoms and did not go into current treatment options.
Corrine Y. Jurgens, PhD, the Chair of the scientific statement writing committee of the AHA described the reason for the publication of the review as follows.
“Symptoms of these cardiovascular diseases can profoundly affect quality of life, and a clear understanding of them is critical for effective diagnosis and treatment decisions. The scientific statement is a ‘state of the science’ compendium detailing the symptoms associated with CVD, similarities or differences in symptoms among the conditions, and sex differences in symptom presentation and reporting.
“Some people may not consider symptoms like fatigue, sleep disturbance, weight gain, and depression as important or related to cardiovascular disease. However, research indicates that subtle symptoms such as these may predict acute events and the need for hospitalization. A broader definition of what constitutes an ‘important’ symptom is warranted.
“Establishing a baseline symptom profile for an individual and tracking symptoms over time may be helpful to detect changes and any progression of symptoms.”
The six CVD entities and their principal symptoms
Heart attack. The formal medical term for a heart attack is “acute myocardial infarction,” “acute” meaning that it occurs suddenly, “myocardial” meaning that it affects the heart muscle, and “infarction” meaning severe injury or death to the tissue, in this case the heart muscle, due to an interruption in the oxygen supplied by the blood. A heart attack is usually referred to as “an AMI” or just “an MI.”
"reveal" emails? If not,
just click here...
Heart attacks fall under the broad category of acute coronary syndrome (ACS), a term that refers to any heart condition caused by sudden loss of blood flow to the heart. The ACS category also includes unstable angina, which is the term for sudden, unexpected chest pain or pressure, even when totally at rest. Chest pain experienced when exercising is called “stable angina,” and is not considered an acute coronary syndrome, but it can progress to unstable angina.
The most frequently reported symptom of ACS, particularly heart attack, is chest pain, often described as pressure or discomfort, and it may radiate to the jaw, shoulder, arm, or upper back. The most common co-occurring symptoms are shortness of breath, sweating or a cold sweat, unusual fatigue, nausea, and lightheadedness. Sometimes these other symptoms are called “atypical,” however, it has been pointed out that labeling these as “atypical” may be the result of the general absence of women from the clinical trials that were the source of the symptom list. Women are much more likely to report those “co-occurring” symptoms than men.
A brief digression: Doc Gumshoe doubts that men experience those “co-occurring” symptoms less frequently than women. There is no basic physiologic reason that men should not experience those symptoms. My guess is that men – stoic and heroic – simply ignore them.
Heart attacks are further divided into two categories, depending on whether an electrocardiogram (EKG) test can detect the event by observing the ST segment of the EKG pattern. The ST segment occurs immediately after the segment which traces the rapid change in electric potential when the heart contracts and pumps out blood. Normally, it returns to the range where it was before the heart contraction, but in severe heart attacks, the ST segment does not return to that range, indicating that the coronary arteries are fully blocked for a significant span of time. Such a heart attack is termed an “ST- elevation myocardial infarction” or “STEMI.”
In some milder heart attacks, the ST segment does return to its original range. That means that the coronary arteries were not fully blocked or blocked for a short time. Those heart attacks are termed “Non-ST-elevation myocardial infarctions” or NSTEMIs. Since an NSTEMI produces no characteristic EKG signal, they cannot be detected by an EKG. However, both STEMI and NSTEMI attacks can be detected by means of a simple blood test for troponin I, a protein that dwells in the heart muscle cells and is released when those cells experience damage, as in a heart attack. Blood tests for heart attacks formerly tested for creatine kinase (CK), but CK is also released from muscle cells after strenuous exercise, potentially leading to false positive tests. Troponin I dwells in heart muscle cells only, and the troponin I test is not susceptible to false positives. Test results are available in about one hour and the test is sensitive for at least a week and sometimes longer.
The most common causes of heart attacks are obesity, lack of physical activity, smoking, and an unhealthy diet. A history of cocaine use has also been linked with increased risk of heart attacks. Some conditions that are known to precede heart attacks are diabetes, hypertension, and elevated levels of cholesterol.
The particular condition that those named common causes leads to is arterial plaque, a condition in which cholesterol is deposited in the walls of the arteries.
Since the mid 1990s, elevated cholesterol was confirmed as the essential cause of coronary artery disease. It had been established that atherosclerosis consisted of cholesterol deposits in the arteries, and the recent 4S trial had conclusively shown that in patients with heart disease, statin treatment greatly reduced the incidence of significant cardiac events such as heart attacks and obstruction of coronary arteries.
Some data got in the way of this unitary explanation. One was that a certain number of individuals who had “normal” cholesterol levels nonetheless experienced the same kind of cardiac events. Paul Ridker, a cardiologist at Brigham and Women’s hospital and Harvard Medical School, found that these persons, who did not have cholesterol at levels that had been associated with heart disease, did have elevated levels of C-reactive protein (CRP), which for more than 80 years has been known to be associated with generalized inflammation.
At about the same time, another Brigham and Women’s/ Harvard cardiologist, Peter Libby, learned that cholesterol didn’t just swim around in the bloodstream. It actually worked its way into the arterial wall. This appeared to constitute a kind of insult to the arterial wall and provoked an inflammatory response, which in turn resulted in the formation of blood clots. It was these blood clots that, at least in some cases, blocked coronary arteries, causing heart attacks, and also blocked cerebral arteries, causing strokes. Peter Libby coined the term “vulnerable plaque” for plaque affected by inflammation that was prone to clot formation.
Paul Ridker followed up his discovery about CRP with a study in which it was shown that treatment with statins not only lowered cholesterol levels, but also lowered levels of this inflammation marker. And in 2008, Ridker presented the results of the JUPITER trial at the New Orleans meeting of the American Heart Association. That trial, in nearly 18,000 subjects with normal cholesterol levels but elevated levels of CRP, found that rosuvastatin lowered levels of CRP and reduced the incidence of signal cardiac events consisting of nonfatal myocardial infarction, nonfatal stroke, unstable angina, or death from cardiovascular causes.
A general conclusion from this data is that elevated cholesterol and elevated CRP as a sign of inflammation are both singly and together significant risk factors for heart attacks and acute coronary syndromes.
Heart failure. As the name implies, heart failure is the general term for a condition in which the heart is not doing its job, which is to pump enough blood into the circulatory system to provide necessary oxygen for all body functions. Here’s what the AHA says about heart failure:
“Shortness of breath is a classic symptom of heart failure and a common reason that adults with heart failure seek medical care. However, early, more subtle symptoms should be recognized as signs to consult with a health care professional. These symptoms may include gastrointestinal symptoms such as upset stomach, nausea, vomiting, and loss of appetite; fatigue; exercise intolerance (related to fatigue and shortness of breath); insomnia; pain (chest and otherwise); mood disturbances (primarily depression and anxiety); and cognitive dysfunction (brain fog, memory problems).
“Women with heart failure report a wider variety of symptoms, are more likely to have depression and anxiety, and report a lower quality of life compared with men with heart failure. Just like with heart attack, women are more likely than men to report different symptoms. In heart failure, women report nausea, palpitations, and digestive changes, as well as higher intensity levels of pain (in other areas of the body, not just chest pain), swelling, and sweating.”
The emphasis should be on reporting those symptoms; we brave men may just be keeping those symptoms to ourselves.
The AHA review said nothing about the underlying causes of heart failure. There are many, many possible causes. Just as the heart provides oxygen-supplying blood flow to all parts of the body, any disease or condition that interferes with circulation and blood flow to the heart can lead to heart failure. Here’s a list:
Coronary artery disease
Cardiomyopathy (a disorder of the heart muscle)
Congenital heart disease
Heart attack
Heart valve disease
Certain types of irregular heart rhythms
Hypertension
Emphysema,
Untreated sleep apnea
Diabetes
Overactive or underactive thyroid
HIV
Severe anemia
Chemotherapy
Drug abuse
Either or both of the heart’s ventricles can be affected by heart failure. When the left ventricle stops pumping efficiently, it fails to send blood via the arteries to all the parts of the body that require oxygen, with the result that their function is adversely affected. The blood that the left ventricle fails to pump into the circulatory system backs up into the lungs, impairing respiratory function.
The right ventricle’s function is to send the blood that has been returned from the venous system into the lungs to collect oxygen. Right ventricle failure is usually preceded by left ventricle failure, with the result that the right ventricle is trying to pump blood into the lungs that are already filled with blood due to back up from the left ventricle. Since the lungs cannot accommodate the blood from the right ventricle, the venous system retains the blood, which can cause severe swelling in the extremities and the lower body.
As with heart attacks and – as we’ll see – other types of CVD, several behaviors tend to increase the risk of heart failure. The list is familiar: smoking, obesity, lack of physical activity, a diet that includes too many saturated fats or trans-fats.
Treatment for heart failure is based on identifying the cause. If the cause is a blocked artery, the appropriate treatment may be bypass surgery, where the surgeon removed the section of the artery that contains the block and replaces it with a piece of healthy artery, harvested from another part of the body.
Other means of opening a blocked artery include percutaneous coronary intervention, in which a surgeon can guide a small balloon or a stent to the blocked area of the artery. Inflating the balloon opens up the artery, while a stent also pushes open the artery. Neither procedure requires open surgery – the balloon or the stent is inserted into an artery near the surface and carefully maneuvered into place.
When a cause of heart failure is an irregular heart rhythm, a likely intervention is the implantation of a pacemaker, which emits electrical impulses that trigger heart beats at a pace that results in sufficient oxygen supply to the body.
Some persons with heart failure benefit from an implantable cardioverter defibrillator, which keeps track of the heart rate and delivers an electric shock that restores the heart rate back to a normal rhythm. This device is suggested for people with an ejection fraction (how much blood the heart pumps out with each contraction) less than 35% if not due to blockages and less than 30% if due to blockages.
Medications are prescribed for heart failure, again depending on the cause. Most classes of drugs for the treatment of high blood pressure are used for heart failure, as are blood thinners, cholesterol-lowering agents, drugs used to treat diabetes, and heart stimulants.
Heart valve disease. The heart is a pump that takes in blood that has given up its oxygen load, pumps it to the lungs to have the oxygen replenished, then takes in the oxygenated blood from the lungs, and pumps it out into the body. Each of these four actions is regulated by a valve that keeps the blood circulating in the right direction. The valves themselves are little flaps of very strong tissue that permit the flow of blood in one direction only. The flaps spread apart to permit the blood flow in the right direction, and then close down to prevent regurgitation.
Oxygen-depleted blood from the venous system flows into the right atrium of the heart. It then flows through the tricuspid valve to the right ventricle. The right ventricle pumps the blood through the pulmonary valve and into the lungs, where it absorbs oxygen. The oxygen-rich blood then flows to the left atrium. The heart pumps blood through the mitral valve into the left ventricle. From the left ventricle, the blood flows through the aortic valve to the rest of the body.
The kinds of heart valve problems include valves that become stiff and too narrow (stenosis), fail to close properly allowing regurgitation (prolapse), or are improperly formed (atresia). Valve disease can also cause pulmonary hypertension. One of the most serious and common forms of valve disease is aortic stenosis, which occurs when the aortic valve narrows and restricts blood flow from the heart.
Women with aortic stenosis more frequently report shortness of breath, exercise intolerance, and physical frailty, than do men. Men with valve disease are more likely to report chest pain than women with valve disease. (This is an instance where the symptom difference between men and women may have some basis in fact.)
Stroke. A stroke is an acute event that requires emergency intervention. The cause is a sudden interruption of blood circulation to an area of the brain, when a blood vessel is blocked by a blood clot, or when a blood vessel ruptures. Strokes caused by the interruption of the blood supply are called “ischemic” strokes, while those caused by the rupture of a blood vessel are called “hemorrhagic” strokes. Ischemic strokes are more common, accounting for about 80% of stroke cases.
It is important that the public at large be able to recognize stroke symptoms so as to be able quickly to get necessary help. The American Stroke Association recommends that the general public should learn and remember the acronym FAST. F stands for Face drooping, A for Arm weakness, S for speech difficulty, and T for Time to call 911.
Other symptoms of stroke are confusion, dizziness, loss of coordination or balance, and changes in visual perception. Recognizing stroke symptoms is critical since immediate treatment may help prevent death or reduce the chance of long-term disability.
According to the AHA, women experiencing a stroke are more likely than men to have other, less familiar symptoms in addition to the common ones. These symptoms include headache, altered mental state, coma or stupor. A stroke may also impair thinking, which may, in turn, impact the stroke victim’s ability to recognize new or worsening symptoms.
After a stroke, some symptoms may linger and require continued care. Treatment after the immediate emergency treatment focuses on preventing these symptoms from becoming disabilities. Post-stroke screening should include assessment for anxiety, depression, fatigue and pain. Pain after a stroke may take months, usually four to six months, to develop.
Strokes are the second leading cause of death worldwide, with an annual mortality rate of about 5.5 million. And about half of stroke survivors have some form of chronic disability. As the global population ages, the public impact of strokes will increase. In less developed parts of the world, most stroke cases occur in persons less than 60 years of age, while in developed countries strokes mostly occur in older persons, 70 years or higher. High blood pressure is the single strongest risk factor for strokes; persons with hypertension are three to four times more likely to have strokes. Illicit drug use increases the risk of strokes.
The recommended practices to minimize the chances of experiencing a stroke as essentially the same as those for avoiding a heart attack, emphasizing diet, exercise, keeping excess weight off, avoiding smoking, being careful with alcohol, and watching blood pressure.
Rhythm disorders. Here’s what the AHA said about rhythm disorders:
“Rhythm disorders, called arrhythmias, are often described as the feeling of an abnormal heartbeat or palpitations that may be irregular, fast, fluttering or halting. Other symptoms include fatigue, shortness of breath, and dizziness, all of which are shared with other cardiovascular diseases. Less commonly, chest pain, dizziness, fainting or nearly fainting, and anxiety may occur in some people with heart rhythm disorders.
“Women and younger adults with rhythm disorders are more likely to experience palpitations, while men are more likely to experience no symptoms. Older adults are more likely to experience either uncommon symptoms or no symptoms. Differences in symptoms have also been found among people from diverse racial and ethnic groups. Data indicate black adults report experiencing more palpitations, shortness of breath, exercise intolerance, dizziness, and chest discomfort in comparison to people who are Hispanic or white.”
If you’re interested in arrhythmias beyond what the AHA had to say, you might look at a posting from Doc Gumshoe on November 20, 2016, entitled “When Your Ticker is Marching to the Beat of a Different Drummer.” In that piece, I described our two nervous systems – the sympathetic and parasympathetic nervous systems – which alternate control over many of our functions, including heart rhythm, between our waking and sleeping state, and how impulses from those systems can lead to arrhythmias.
There are several different types of arrhythmias. Tachycardia is a rapid heartbeat, 100 beats per minute (bpm) or more. That heart rate is easily attained through vigorous exercise, but fever also increases the heart rate. It increases about 10 bpm for every degree Fahrenheit over the normal 98.6⁰ mark; translated to the Celsius scale, that’s 18 bpm for every degree over the 37.6⁰ mark.
Bradycardia describes a heart rate less than 60 bpm. In athletes and individuals with exceptionally strong hearts that pump out greater volume of blood with each beat, requiring less frequent contractions to maintain optimum perfusion, a slow heart rate is normal. However, events or stimuli that trigger a response by the parasympathetic nervous system can result in release of acetylcholine by the vagus nerve, slowing the heart rate.
Premature contractions can result from electrical impulses generated from other places in the heart other than nodes that keep the whole organ marching to the same beat. These are called ectopic foci, and the usual causes are small areas of ischemia or calcification and toxic irritation, such as from drugs, caffeine, or nicotine.
Atrial fibrillation is one of the more common arrhythmias, which can occur as a fairly consistent condition or only on occasion. In most cases, atrial fib is a relatively benign condition, but there are some consequences of concern. Atrial fib can reduce overall cardiac output, causing fatigue. Also, when episodes of atrial fib are over, there can be a marked pause before the next contraction, which in some cases can result in syncope, or fainting. But by far the most common concern is that the inefficiency of the atrial contraction leaves blood pooling in the atria, possibly resulting in clot formation, which can travel to a spot in the body where it can do significant harm.
Ventricular fibrillation is the single most serious cardiac arrhythmia, which, if not rapidly resolved, is fatal within a few minutes. In ventricular fib, some sections of the ventricular muscle are contracting while others are relaxing. The ventricles stop pumping blood, and within a few seconds a person loses consciousness because of lack of blood to the brain. Death follows in a few minutes, unless the fibrillation is reversed. Ventricular fib is probably the single most common cause of fatal cardiac arrest. One cause of ventricular fib is electric shock from a 60 cycle alternating current, which is our usual house current. Other than external electric shock, the most common cause of ventricular fib is ischemia of the heart muscle or of the specialized cardiac conducting system.
The most effective intervention for ventricular fibrillation is external electric shock defibrillation. The heart stops completely for a few seconds, and then the normal sinus rhythm can return. Defibrillators, such as those that are carried by emergency medical personnel, deliver a single shock of several thousand volts for about one thousands of a second. If defibrillation takes place very quickly after the onset of ventricular fibrillation, the heart will usually return to its normal rhythm. But if ventricular fib has been going on for much longer than one minute, the heart may be too weak from lack of oxygen to resume beating on its own, in which case cardiopulmonary resuscitation will be required.
Vein and artery disease. The usual term for this is peripheral vascular disease; the AHA describes the symptoms of vein disease and artery disease separately.
Peripheral vein disease does not necessarily cause any symptoms, but it may cause leg pain and achiness, with heaviness or tightness in the legs. Fatigue, cramping, restless leg syndrome, and skin irritation have been observed. In one study, according to the AHA, adults younger than age 65 were more likely than older adults to report pain, heaviness, achiness, and fatigue. Symptoms of vein disease sometimes occur even when there are no visible signs of the condition.
Peripheral artery disease (PAD) leads to reduced blood supply to the legs. The classic symptom is pain in one or both calf muscles that occurs while walking and subsides with rest. This is called claudication. However the most common symptoms of peripheral artery disease are pain in other parts of the legs and in the feet and toes rather than calf pain. PAD with symptoms is associated with an increased risk for heart attack and stroke, with men at higher risk than women.
The most common cause of peripheral vascular disease is the buildup of plaque inside the artery wall, which reduces blood flow, decreasing oxygen and nutrients to the tissue, and potentially leading to clot formation, which can clog arteries. Clot formation in the arteries that supply blood flow to the legs can have much the same effect as clot formation in the coronary arteries.
Other possible causes of peripheral vascular diseases may include injury to the arms or legs, anatomical irregularities, or infections.
Some of the risk factors that have been cited for heart attacks and strokes are also risk factors for peripheral vascular disease, namely hypertension, obesity, physical inactivity, and smoking. Elevated cholesterol levels and diabetes are also linked with peripheral vascular disease.
The AHA statement emphasized the importance of depression as a factor in cardiac disease. National survey data shows that people with cardiac disease have about twice the rate of depression compared to people without any medical condition (10% vs. 5%). According to the AHA, depression should be considered a risk factor for worse outcomes after an acute coronary syndrome event or diagnosis.
Corrine Y. Jurgens, speaking for the AHA, had this to say in summary:
“Symptom relief is an important part of managing cardiovascular disease. It is important to recognize that many symptoms vary in occurrence or severity over time, that women and men often experience symptoms differently, and factors such as depression and cognitive function may affect symptom detection and reporting. Monitoring and measuring symptoms with tools that appropriately account for depression and cognitive function may help to improve patient care by identifying more quickly people who may be at higher risk.”
The AHA’s emphasis on recognizing heart disease symptoms reflects a basic fact about heart disease, which is that by far the most effective way to protect people from the severe and often fatal consequences of heart disease is prevention rather than treatment. Prevention requires a focus on early recognition of symptoms. It makes no sense to wait until the person has a heart attack and then hope that some miraculous treatment will repair the damage. The very substantial progress that has been made in reducing the rate of heart attack and stroke fatalities has been the result of identifying the risk factors and taking steps to attempt to tamp them down. Those steps constitute treatment for cardiovascular disease, of course. And, while that progress should be acknowledged, there is yet much to be done in addressing cardiovascular disease, which has become our most significant threat.
* * * * * * *
At the same time that Doc Gumshoe was looking into the cardiac diseases, there were other happenings on the healthcare front, which will be discussed in the next epistle. I will also address some of the comments that you kindly submitted. Enjoy Thanksgiving, if I don’t get back to you before then! Thanks, Michael Jorrin, (aka Doc Gumshoe)
[ed note: Michael Jorrin, who I dubbed “Doc Gumshoe” many years ago, is a longtime medical writer (not a doctor) and shares his commentary with Gumshoe readers once or twice a month. He does not generally write about the investment prospects of topics he covers, but has agreed to our trading restrictions. Past Doc Gumshoe columns are available here.]
Cholesterol does not generally cause heart attacks. Your body makes over 80% of it’s own cholesterol and a small percentage comes from the diet. Cholesterol is in every cell of the body. Just as many people with low cholesterol die of heart attacks as with high cholesterol. Inflammation of the endothelium, is a much more likely culprit along with nitric oxide issues.
Agree! I am grateful for the up to date, accurate depiction of cholesterol and the role it plays in our bodies at the cellular level. We need it! All this statin usage does more harm than good for many who take them.
I agree. There is a theory that cholesterol plaques are the body’s attempt to deal with coronary arteries that have become damaged and inflamed by irritants such as cigarette smoke contaminants and/or alcohol in the blood.
So long as practitioners continue to view the heart as a pump there will be little meaningful progress. It is a vortex generator. The aorta arches more acutely as blood spirals into it from the left ventricle, whereas it should straighten if the pump hypothesis were true. Then, how can a pump with a power output of only 1-2 watts pump several liters of blood through 100 km of blood vessels of varying size, the smallest of which, the capillaries, being narrower than the red blood cells themselves? No, as with so many things, allopathic medicine has got it all wrong. I see no mention here of modern vaccine technologies and their adverse effects on the heart. Then, in the CVD mortality table, France and Japan have the lowest frequencies yet both have greater numbers of smokers than many of the other countries for which data are shown. Cholesterol, even the low density variety, has been debunked several times. I could go on but I don’t think this article offers “another look at the heart”; it offers an erroneous upholding of the “conventional view of the heart”.
ps My father died of MI, my sister and her husband have both suffered heart attacks in the last 18 months, and my wife needed to have her aortic valve replaced last year. So, I have given the subject some thought and I find the dogma offered by the medical profession wanting in a great many respects.
To echo Tom, sorry about all those horrible egg white omelets you suffered through, and sorry for the skim milk you drank, and most all, apologies to the dairy farmers who went bankrupt.
Inflammation is the new black.
I couldn’t agree more with John…this is not another look, it is just a regurgitation of the flawed conventional medical dogma! Our medical system is a flawed fraud! If you doubt me, just look at how sick our country is, as compared to how sick it was 50 to 70 years ago…and follow the MONEY!
True, bottom line is without hereditary disease from your parents; you are what you eat and what you don’t do such as exercise! This was a great in-depth article and if you look at obesity rates in the U.S. vs other countries you’ll see how this corelates with our CVD mortality ratios.
I have been hearing a lot about the negative consequences of statin consumption. Has Doc encountered any of this in his research?
A better acronym for Stroke recognition is BE-FAST – which stands for Balance, Eyes, Face, Arms/Legs and Time. I had a blood clot that landed in my left occipital lobe, resulting in the suddenly lost of right peripheral vision in both eyes. It was most likely caused by AFIB due to damage from a heart attack and triple bypass 12 years ago. Fortunately, I received a clot buster drug within a few hours of onset and my vision return to within 99% + of normal.
Excellent article, many thanks. I am trying to find out if I can get free training here in the UK in first aid and the use of a defibrillator.
Well, Michael, your new article is a gut-punch for me. I now am old and fat and in pain, heaps and heaps of pain; the source of my accumulating adiposity. (No details.) I often wonder whether my physical woes are senescence or something more specific; I gave up on my doctor and her interminable battery of tests as they moved ever farther from my pain.
Thanks to your article, I must acknowledge my looming death. I have no such prognosis from any doctor – but I should begin now, stat!, to get my life and finances in order so my wife will not struggle with unclosed financial affairs I leave undone. I prefer she remember me with fondness rather than another wipe of her brow.
Which is one reason I habituate Stock Gumshoe: To invest our portfolio with the goal of increasing its value today, tomorrow… and beyond my death. Thank you.
In many previous Doc Gumshoe postings, I have clearly stated that indeed we do make cholesterol from whatever food we eat, and also that we require cholesterol, since it is an essential component of many bodily functions. And, by the way, I have pointed out that cows make cholesterol from hay. Cholesterol is harmful only when it is deposited in the walls of our arteries, and then only when it is unstable and bits of it break loose and clog coronary arteries. In this posting I took care to point out that inflammation plays a major part in making arterial plaque vulnerable. And I dedicated a previous posting to the role of inflammation.
As for statins causing harm, whatever harm they cause is greatly outweighed by their benefit.
And as for using the term “allopathic medicine” as a despective, the evidence supporting that form of medicine, which uses drugs as disease treatment (along with other treatment options) is very, very strong.
Robert Lustig wrote a book recently called Metabolical. If Doc Gumshoe would read it, I think it may change his narrative a little bit on Heart Disease and Statins.