The previous Doc Gumshoe piece on the subject of sleep, which posted on March 19 (“Sleep: Order and Disorder”), elicited 49 comments, which I was unable to respond to, because my computer went on the blink just a couple of days later. My local computer geek took a few days to restore the computer to health and install the necessary panoply of updates, and I will now attempt to address the issues raised in those comments – to the best of my ability.
But first, an embarrassing admission: the majority of those comments related to the matter of sleep apnea, and I knew very little about sleep apnea. My understanding was that if you had episodes of sleep apnea, you would need this device that would pump air into your lungs – continuous positive airways pressure (CPAP). That is about all I knew about sleep apnea. Therefore I have had to go back to basics and bone up.
I was surprised and more than mildly alarmed to read that one of the respondents had experienced 510 incidents of suspended breathing. This person also noted that sleep apnea could be fatal. This should have been obvious to me – if you stop breathing and do not resume breathing, that’s tantamount to the long goodbye. So sleep apnea is not only bad for our general health, since it deprives us of needed oxygen, but it can be – rarely, thankfully – fatal. It requires serious attention.
Another respondent reported experiencing about 100 incidents of sleep apnea in one hour. This respondent said that sleeping with a mask had been very hard to get used to, but now he/she is feeling great. The CPAP device was life-changing.
Surgical options
One comment mentioned surgery as an option, because any number of seemingly minor abnormalities in the anatomy of the nose and throat can cause interruptions in breathing, which, if they occur while we are sleeping, result in sleep apnea.
A bit of online digging turned up a piece by WebMD, which is usually a reliable source of medical and healthcare related information. The number of surgical options is surprisingly large. The WebMD write-up mentioned several distinct sites of surgical intervention for sleep apnea, including the nose, the tongue, the soft palate, and the bones of the face, neck, or jaw.
I should point out, before digging into the details of these options, that they aren’t one-shot solutions to the problems of sleep apnea. In several cases, it is noted that the individual experiencing sleep apnea may need to continue the use of CPAP or related devices. Surgical intervention prevented anatomical interference with the breathing process, but interruptions of lung activity could still occur, requiring the continuation of continuous positive airways pressure.
The physician first investigates the nose and throat area by means of a nasopharyngoscope, which enters the nasal passage and goes down the back of the throat. This is an uncomfortable procedure, and the patient is given a temporary local anaesthetic.
The nasal passage itself may be blocked by growths called polyps, or by curved bones along the wall of the nose called turbinates. These growths can removed by surgery.
The cartilage and bone that separate the nostrils can be distorted, a fairly common condition known as a deviated septum, which can impair breathing and be a cause of sleep apnea. The surgery that corrects this condition is called septoplasty.
The soft tissue in the roof of the mouth (the soft palate) and around the sides of the throat can clog the airway during sleep and cause sleep apnea. This can be addressed by surgery. Palate surgery, technically called by the tongue-twister name uvulopalatopharyngoplasty (UPP), is one of the most common surgeries for obstructive sleep apnea in adults. The surgeon removes part of the soft palate, the tonsils, and the uvula. Healing can take 6-8 weeks.
The tonsils and the adenoids are lymph nodes behind the nose or on the sides of the throat. One or both can swell up and block your airways. Tonsillectomies are frequently performed on children when their tonsils are infected in connection with upper airways infections.
In patients with mild symptoms of obstructive sleep apnea, the physician can use a laser or electric current to zap off parts of the soft tissue. This is termed laser or cautery-assisted uvulopalatoplasty, usually an in-office procedure, generally used in patients with mild symptoms.
Also in patients with mild sleep apnea, the doctor might implant a few small rods in the throat, which will stiffen up the soft palate and prevent it from blocking the airway.
Another way to open the airways is tongue surgery, called a lingual tonsillectomy. The doctor removes tissue from the base of the tongue or pulls the tongue muscle forward and attaches it to the chin bone. This surgery is called a genioglossus advancement.
Hypoglossal nerve stimulation (HNS) uses electricity to make breathing easier. The physician places a small device under the skin on the chest. The device resembles a pacemaker, but the wires attach to a nerve that controls the tongue muscle. During sleep, an electric signal can trigger this nerve to push the tongue forward, preventing it from blocking the airways.
HNS may be recommended for sleep apnea patients who are unable, for any reason, to use a CPAP device. It cannot be used if the patient is under 22 years of age or has a BMI greater than 35.
HNS is not recommended for persons with a concentric collapse in the airway, meaning that the soft tissue in the roof of the mouth and throat close in on all sides during sleep.
In some patients with sleep apnea, the cause is the formation of the jaws. Sometimes surgically moving the jaws forward opens up the throat and makes breathing easier during sleep. This procedure is called maxillomandibular advancement (MMA). There’s some evidence that MMA works better than other surgeries for sleep apnea such as UPP, but it’s riskier and requires longer recovery – three to five days in the hospital, with the jaws wired shut.
A last-resort option might be a permanent tracheostomy, a procedure in which the surgeon makes a small opening in the trachea (i.e., the windpipe). During sleep, patients who experience this procedure are able to breathe through a tube that fits into that opening. The tracheostomy can be capped during waking hours, so that the patient can breathe and speak normally.
The number and variety of surgical and semi-surgical options was surprising to me, although, considering the prevalence of sleep apnea and the non-trivial chance that it could be fatal, I should not have been surprised.
"reveal" emails? If not,
just click here...
And, as I mentioned earlier, these surgical options do not always make CPAP devices superfluous. Some individuals need surgical intervention and continuing CPAP assistance with breathing during sleep.
Other options
The eXcite OSA
A comment on the previous sleep piece mentioned a device called “eXciteOSA,” from Signifier Medical Technologies. I see that it was FDA-approved on February 5, 2021 to reduce snoring and mild obstructive sleep apnea.
It is used during waking hours for about 20 minutes per day during a wakeful state. The device works by delivering electrical muscle stimulation through a mouthpiece that sits around the tongue. It is intended to improve tongue muscle function, which in time can help prevent the tongue from collapsing backwards and obstructing the airway during sleep.
The mouthpiece has four electrodes, two located above the tongue and two located below the tongue. It provides electrical muscle stimulation action in sessions that consist of a series of electrical pulses with rest periods in between. It is used for 20 minutes once a day, for a period of 6 weeks, and once a week thereafter.
The eXciteOSA device is not intended for patients who have or are suspected of having moderate or severe sleep apnea with an apnea-hypopnea index of 15 or higher, hypopnea being the term for shallow or restricted breathing, but not stopping breathing altogether. The apnea-hypopnea index (AHI) is the combined average number of apneas and hypopneas that occur per hour of sleep. According to the American Academy of Sleep Medicine (AASM) it is categorized into mild (5-15 events/hour), moderate (15-30 events/hr), and severe (> 30 events/hr). I should note that the validity of the AHI as a measure of the severity of sleep breathing issues has been questioned in the medical literature, but no alternative measure has emerged in its stead.
The Herbst Appliance
This is a device that repositions the jaws, bringing the lower jaw into a more forward position, which is better for alignment of the teeth. It has been in use in orthodontic dentistry, and has been modified for use in sleep-disordered breathing. According to the manufacturer, the Herbst Appliance permits lateral and vertical movement while maintaining the desired mandible-forward position. It is sturdy and fully adjustable to find the most effective and comfortable position. Adjustment of position is quick, easy and very accurate.
The Herbst Appliance is one of ten devices marketed by Aspen Ridge Sleep Solutions.
As I poked around in Google for sleep apnea treatment options, I was dumfounded by the immense number of options. For example, inputting “sleep apnea treatment” produced 99,700,000 results one time, and different huge numbers other times. What that tells us is that there are huge numbers of persons who are experiencing sleep apnea, or who suspect that they have this condition.
Just for drill, I questioned Google once again about sleep apnea options. This time the answer was 76,400,000. Where did those other 23,300,000 go? Search me!
Needing to be awake and alert versus needing to get a good night’s sleep
Most of us turn to caffeine, whether in coffee or tea or some kind of medication, to feel awake. What does caffeine do? The chief mechanism of caffeine is to dial down the activity of a neurotransmitter called adenosine. Adenosine plays a number of different roles in the body, and the adenosine phosphates – mono-, di-, and tri-, or AMP, ADP and ATP – are central to our metabolism. In the brain, one of the things adenosine tends to do is put a sort of damper on some forms of neuronal activity – in other words, it quiets down the brain and permits us to go to sleep. Caffeine blocks adenosine receptors, inhibits that quieting effect, and helps keep us alert and awake.
The effects of caffeine vary considerably among members of our species. I, for one, rely on my morning coffee to get me going (although that might be a kind of placebo effect – it’s the blissful aroma of that blend of several kinds of coffee that starts my day). But I can usually drink a double espresso after dinner and sleep the sleep of the just. My wife, however, is reluctant to drink any coffee at all much past noon lest she have a problem falling asleep.
Which takes us to the dilemma of shift-workers, who may work during the night-time hours and need to sleep during the day. If they rely on coffee or caffeine in any form to stay alert during their shifts, how long will it be before they feel dozy and relaxed?
Perhaps because of the unpredictability of caffeine, many people employ other strategies to stay awake, whether for shift work, studying, driving, or any other activities. We will avoid discussing the extreme cases, since after all our principal focus in this piece is sleep, and not staying awake. In passing, we should acknowledge the use of amphetamines and similar agents that are primarily intended for the treatment of attention deficit disorder, e.g., Adderall, Ritalin, Vyvanse and the like. Short-acting formulations of these drugs may be used to keep a person awake and alert without carrying over and seriously interfering with sleep time. The abuse of these drugs is widely recognized, and is related to what many consider the over-diagnosis of ADD and ADHD – which is another subject for another time.
However, the need for something that helps people stay awake brings me to a drug, with an entirely different mechanism of action, which, as it happens, may also be employed to help people get good sleep.
Modafinil and orexins
Modafinil (Provigil, Alertec) and armodafinil (Nuvigil), both from Cephalon, wholly owned by Teva Pharmaceuticals, are relatively new stay-awake drugs that have gotten a great deal of attention lately. Modafinil was FDA approved for narcolepsy in 1998 and for shift-work sleep disorder in 2003. Armodafinil is the R-enantiomer of modafinil, meaning that it consists of only the right-handed version of the molecule (thus R-modafinil or armodafinil) . In many instances, the effectiveness of a drug depends on the precise shape of the molecule, and the precise way it locks with its targets. Two molecules can have the identical chemical composition, but be exact mirror images of each other. One locks with the target while the other does not. Think of the way a key fits into a lock: it can be cut in the same way, but if the grooves are on the wrong side, it will simply not go into the lock. Modafinil is the so-called racemic compound, consisting of both the right- and left-handed molecules, while armodafinil consists of only the molecules that fit the target.
Modafinil (and armodafinil) have been referred to as Viagra for the brain – they are stimulants, and may work by activating neurons called orexins (sometimes also called hypocretins, but we’ll stick with orexins). Orexins extend their axons to various parts of the brain that are involved with wakefulness and attention, and activation of orexins increases the levels of dopamine and norepinephrine in those areas. Norepinephrine in particular is the neurotransmitter that stimulates waking physiologic functions such as heart rate, lung capacity, energy production, and muscle strength. So far, these agents have not demonstrated much risk for abuse, unlike the amphetamines and other stimulants, which are commonly abused.
The side effects of any stay-awake medication are difficult to separate from the inherent effects of not getting enough sleep. The most frequent adverse event in clinical trial patients taking modafinil was headache, experienced by 34%; however, 23% of patients taking placebos also experienced headaches. Most other adverse effects were in the single digits.
What is particularly interesting about modafinil is that it gives us insight into the connection between orexins and sleep. If activating orexins can help promote wakefulness, would it not be possible that blocking the activity of orexins would promote sleep?
Sleep promoting mechanisms
Most sleep medications have worked by means of the neurotransmitter gamma-aminobutyric acid, or GABA, which is the chief inhibitor of neurons. The drugs that had this effect were discovered long before the identification of the mechanism. It was found that barbiturates induced sleep; only later was the inhibitory mechanism of GABA identified and studied. Barbiturates, such as Phenobarbital, Seconal, or Veronal, really do induce sleep. They do this by greatly slowing all transmission of signals in the cortex. Their defects are well known, including a tendency to be addictive; the celebrities who were hooked on barbiturates are many and notorious, e.g., Marilyn Monroe. And there is a tendency to overdose. It’s not easy to get the dose just right; people wake up sooner than they want to, or else they wake up feeling drugged.
Several other classes of sleep-inducing drugs also addressed GABA receptors, even though they may have different mechanisms of action. These include the benzodiazepines, such as Ativan (lorazepam), Dalmane (flurazepam), Halcion (triazelam), Restoril (temazepam), and others. These agents have a somewhat different effect than the barbiturates; their goal, rather than knocking you out, is to ease you into sleep by quieting down your anxieties. As noted earlier, they are primarily anxiolytics. Some people get habituated to drugs of this class; they find that to achieve the desired effect, they have to keep upping the dose. This might be considered a form of addiction.
And some antihistamines induce sleepiness, such as Benadryl (diphenhydramine), Desyrel (trazodone) and others; a major drawback of these is that in some people the effect lingers past the desired sleep period – i.e., you’re dopey the next day.
The blockbuster entry – I am not using that term loosely – was Ambien (zolpidem) from Sanofi, which also targeted GABA receptors. Currently, Ambien and Ambien CR account for about 70% of the 60 million or so prescriptions for sleep medications in the US. However, Ambien’s drawbacks are widely recognized, including a range of erratic behavior that has been widely publicized in the media. Some people take the drug with no intention at all of going to sleep – instead they enjoy a feeling of disinhibition that permits them to engage in all manner of activities, ranging from the merely silly (gorging on cupcakes) to the genuinely risky (reckless driving).
Ambien’s problems have led the FDA to issue a number of warnings and also reduce the dosage. In the meantime, Sanofi has introduced a controlled release formulation (Ambien CR) that is meant to offset one of Ambien’s problems, namely, that it is a relatively short-acting drug. Ambien tends to put people to sleep, but it’s not so good at keeping people asleep. The CR formulation releases the drug into the system over a longer period.
The way Ambien induces sleep might be compared with stopping a machine by filling the works with a dense, sticky liquid. Addressing the orexin system is a fundamentally different mechanism. Orexins promote wakefulness; thus, an orexin antagonist is like pressing the snooze button on the alarm clock. Or, to return to the machine analogy, it stops the machine by simply interrupting the power supply.
Suvorexant (Belsomra): an orexin antagonist
This drug, from Merck, was approved by the FDA in 2014. It was approved on the basis of three Phase 3 clinical trials in more than 500 subjects, including individuals who had been diagnosed with primary insomnia. Sleep-lab results demonstrated that the subjects taking the active drug did actually spend more time in slow-wave sleep than did patients taking the placebo; their subjective perception of how much sleep they were getting didn’t differ a great deal, but the sleep-lab data were enough to persuade the FDA to approve the drug for the treatment of insomnia.
Suvorexant has also been studied, with encouraging results, in patients with chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea.
An important difference between Belsomra (suvorexant) and Ambien (zolpidem) is that Belsomra does not result in feelings of euphoria or disinhibition – it just shuts off that internal alarm clock without giving people that Ambien joy ride.
But, speaking of joy rides, it does appear to be the case that subjects who had taken suvorexant did demonstrate impaired driving upon waking up; this has prompted the FDA to issue the usual caution against driving or “engaging in activities requiring full mental alertness” subsequent to taking the drug.
There was a lengthy back-and-forth between Merck and the FDA on the matter of dosage. Because there is a very big placebo effect in clinical trials with sleep medications, the dose of the active drug in the clinical trials has to be big enough to elicit a clear distinction between active drug and placebo. Merck tested dosages from 10 mg to 80 mg, and was leaning towards making 40 mg the standard dose. But because of side effect concerns – impaired driving and others – the FDA has approved four dose levels – 5 mg, 10 mg, 15 mg, and 20 mg, with the 10 mg dose being standard. Merck scientists have expressed the view that the 10 mg dose would not be an effective anti-insomnia medication, but Merck is clearly taking what it can get and hoping to push the standard dose higher.
Suvorexant is the first orexin antagonist; certainly others are on the way. The advantages of employing that pathway to treat sleep problems are many, and the market for sleep aids is enormous. Suvorexant has the potential to be a dominant drug for Merck – I would even consider using the “B” word – “blockbuster!”
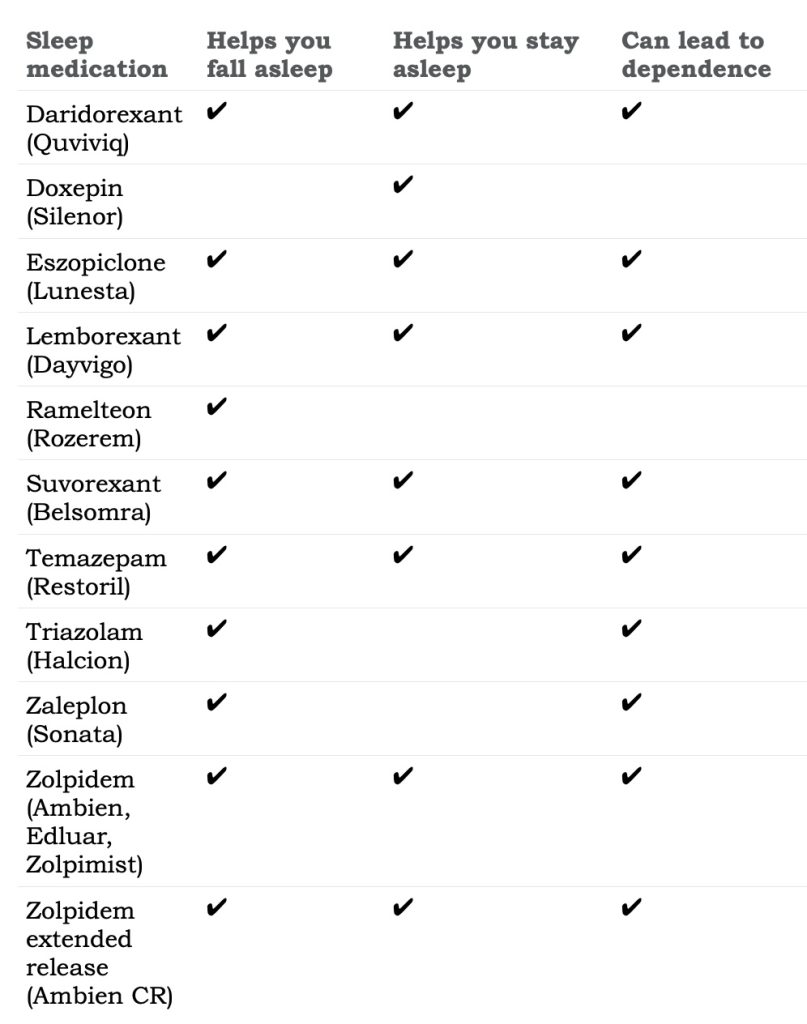
Here is a list of current prescription sleeping pills, courtesy of the Mayo Clinic:
Other options
From Doc Gumshoe’s perspective, a first step in addressing sleep problems is to try to figure out just what it is that’s keeping you awake and try to deal with it. The W. C. Fields advice to insomniacs – “Try to get a lot of sleep” – is clearly counterproductive; the very act of trying keeps you awake. A boring book before turning out the light might help; or hot bush tea, perhaps with a spoonful of honey and a dollop of rum. But what prevents lots of people from sleeping soundly and long enough is that they aren’t able to put the brakes on their busy brains, which keep speeding along and exploring different paths. My personal view on this is that it’s useless to try to tell your brain what to do – that only makes it more obstinate and willful. Let it go along whatever pathways it wants to take, and before long it begins to drift and not make too much sense, and there you are, right where you want to be – in the arms of Morpheus.
A bit more about dreams
An article in the science section of the New York Times caught my attention. (“Vital Activity Takes Flight in Their Dreams,” Maria Popova, 03/26/2024) It was about the likelihood that birds also had dreams. This was based on functional MRI studies of bird brains, which provided convincing evidence that the areas of the brain that controlled flying were active while the birds were asleep. The article also pointed out that birds slept quite differently from most other animals – with one eye open, for example. The article suggested that bird’s brains were where REM sleep – when dreams occur – first manifested, from an evolutionary standpoint.
But what particularly struck me in that article was what it said about the role dreams played in human thought and creativity.
“. . . the bird brain might be where evolution designed dreams – that secret chamber adjacent to our waking consciousness where we continue to work on the problems that occupy our days. Dmitri Mendeleev, after puzzling long and hard over the arrangement of atomic weights in his waking state, arrived at his periodic table in a dream. ‘All the elements fell into place as required,’ he recounted in his diary. ‘Awakening, I immediately wrote it down on a piece of paper. Stephen Alexander, a cosmologist now at Brown University, dreamed his way to a ground-breaking insight about the role of symmetry in cosmic inflation that earned him a national award from the American Physics Society. For Einstein, the central revelation of relativity took shape in a dream of cows simultaneously jumping up and moving in wavelike motion.”
You will notice, perhaps, that I have not – so far – said one word about nightmares. My guess is that nightmares fall into that category where “I’d rather dream about it than have to face it in reality.” They serve a purpose, as do our dreams. It all fits in, somehow or other.
*****
Next up, back to keeping up with developments in the healthcare front, from treating drug addiction with psychedelics to Alzheimer’s and chronic fatigue syndrome. And, just to keep current, what’s the current state of the COVID-19 pandemic, if we still want to call it by that name. Do please stay well, enjoy Spring (whenever it finally appears), and keep those comments coming! Thanks, Michael Jorrin (aka Doc Gumshoe)
[ed note: Michael Jorrin, who I dubbed “Doc Gumshoe” many years ago, is a longtime medical writer (not a doctor) and shares his commentary with Gumshoe readers once or twice a month. He does not generally write about the investment prospects of topics he covers, but has agreed to our trading restrictions. Past Doc Gumshoe columns are available here.]
Thanks for the interesting article. However, orexins (or hypocretins) are not neurons, but bioactive peptides that are produced and secreted by some neurons.
Thanks for that fix! I don’t like making dumb goofs & appreciate corrections.
Thanks, Doc. You’re always helpful. I used to have sleep apnea (as did my father), but I more or less solved it by always sleeping on my side with my head propped up on a sturdy pillow.
I tried that for a decade, it didn’t go away but got worse
I was diagnosed with sleep apnea in January. I kinda knew as my wife has been telling me i often stop breathing in my sleep. My sleep test showed something like 12o episodes every night. I have been using the “res med” machine since 1/15/24. The first 2 breathing masks did not work out well, i’ve tried to avoid the one that covers the mouth and nose and haven’t used that one. The one i’m using with best success has 2 small inserts that pump air directly into my nose. Sometimes i wake up with a severe dry mouth because you just can’t open the mouth, that constant air flow dries your mouth within minutes. I am sleeping better, it takes some getting used to but my oxygen levels are higher and i don’t take my afternoon naps as often. I’m assuming my energy levels will increase as well. As it turns out the cost of the res med devise is covered by medicare 100% so nothing but positives so far.
For “cummingbass”, try a product called Xylimelt, available everywhere (I buy mine at WalMart online in the bottle to save $). The tablets have a ‘sticky’ side that you moisten and adhere to your gums – takes just 30 seconds or so. They stay in place and the outer portion lubricates your mouth. I do not use CPAP (perhaps I should?) but developed ‘dry mouth’ from mouth breathing. I put one tab on the upper right and one on the lower left of my mouth and it works great. There are 3 flavors and also come suger-free. I also use a “BreatheRight” nose strip (or generic) and that helps me breathe through my nose instead of my mouth as much.
Doc, great effort at trying to write about a very complex medical issue. As a medical practitioner who treats sleep apnea, I thought I would let you know that the most successful non-surgical treatments are CPAP and oral appliance therapy. And as one of your readers mentioned, sleeping on your side may be very helpful for many. In terms of oral appliance therapy, you mentioned the “Herbst”. I thought you might be interested to know that there are actually over 190 FDA approved oral appliances that can be used to treat sleep apnea, and generally there is not one device that has been proven to work better than another – they all perform the same function of holding your lower jaw forward during sleep to open your airway (similar to the jaw thrust procedure used during CPR). And Herbst’s are made by many labs, not just the one that you mentioned. I recommend that anyone that wants to be treated using an oral appliance use a dentist that has undergone special training in this field – and they should work as a team with your physician.
In terms of surgical procedures, most of them have fairly lack luster success rates (but they certainly can be successful for some), except for hypoglossal nerve stimulation and MMA surgery.
Obstructive sleep apnea is often only partially an anatomical problem and almost always has some neurological component that only occurs during sleep. After all, none of these patients are experiencing awake apnea….the latest research indicates that sleep apnea occurs from a mixture of 4 components – poor anatomy, improper muscle responsiveness, breathing rhythm problems/high loop gain and/or low arousal thresholds.
I hope this helps your readers – you did a great deep dive!
Great summary, Dr Cohn, thank you!
FYI, my wife and I have been fighting sleep apnea for over 20 years–when the first CPAP machines became available and well before the introduction of the more advanced BIPAP machines. For us, the telltale signs were acid reflux, snoring, chest pains and constant fatigue. My wife had the draconian UPP operation. The doctor said it is the most painful operation a human can endure and she would certainly agree. Also, after the removal of a substantial amount of her throat tissue, she has a very hard time swallowing salads and bread. One item I think you forgot to mention is the difference between OSA and CSA. I have Central Sleep Apnea, as my brain “forgets” to tell me to breathe when I sleep. That means no operation will significantly help my situation. Habits that seem to improve our situation are losing weight and avoiding alcohol at night.
Your comment on Google reminded me of something I stumbled on today
https://kagi.com/
Now I have not tried it yet, however I have seen some good reports
https://www.404media.co/friendship-ended-with-google-now-kagi-is-my-best-friend/?action=subscribe&success=true
Just thought I would pass it on.
I use melatonin 2mg which works for me; take it an hour or so before trying to go to sleep for a week and then stop using it. Interesting to note the difference in share price for Resmed.au (where I live) and Resmed.us
You are lucky, melatonin only works for people with mild sleeping issues. If you have anxiety, melatonin will do not nothing without a drug to help the anxiety. Mirtazapine (prescription needed) has helped reduce my anxiety enough so the melatonin will work. But is has side effects also such as sexual delayed ejaculation.
Travis. I feel for you bud. Was in a full restraining neck brace for 8 weeks. Couldn’t look up, down, right or left . Had to wear to bed. I’m paying for all that moto crossing I did for years in my yute. Getting back to your situation with your CPAP gear, have you asked or tried INSPIRE? My son in law loves it. Hang in there bud
Great article, but you may want to mention the anticholinergic burden of some of these drugs, especially considering your next post on Alzheimer’s.
Doc, thanks for your great expansion on the options for treating sleep apnea. FYI, the Herbst appliance you mentioned is also available with a strap that holds down the tongue, so that it can’t fall backwards to block the airway.
Concerning the “busy brain” sleep problem: I used to have this problem. I would get in bed and relax, and find myself thinking of things I need to do, or answers to problems to look at. Once I thought of one, it kept circulating in my brain, as if my mind was worried about forgetting it. So I kept a pad and pencil next to the bed. When one of these items came to me, I jotted it down, telling myself, now I don’t have to think about it because it will be there for me tomorrow. Over time I started printing these short notes to make it easier to read them the following day. This system helped me a lot.
A number of sleep studies have shown that a rocking motion can help induce sleep faster, get to deeper sleep, longer, and even help with memory. No drugs, calming, relaxing. I would encourage you to check it out. Most of the beds to come out have motors and rollers, potentially noisy and jerky. Lullabed.us is a prototype bed that is silent and very smooth. We’re working on bringing it to market.